Omega-3 fatty acids are linked to better lung health, particularly in patients with pulmonary fibros
Essential fats found in fish and nuts are tied to many protective health benefits. Researchers found they may also slow decline of lung function and prolong the lives of pulmonary fibrosis patients.

Omega-3 fatty acids have garnered significant interest among patients and clinicians for their potential protective health effects, including lung health. In our recently published research, my colleagues and I found that higher dietary intake of omega-3 fatty acids is linked to better lung function and longer survival in patients with pulmonary fibrosis, a chronic respiratory disease.
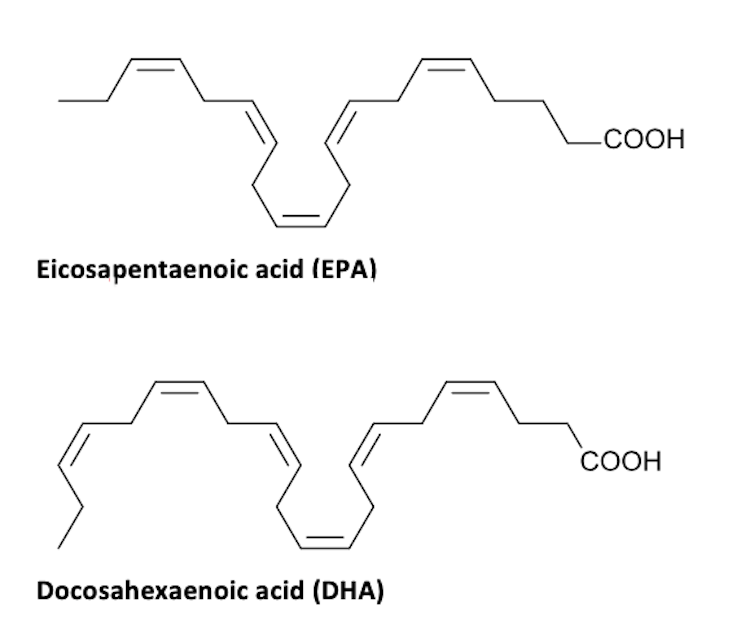
Found in foods such as fish and nuts and in some supplements, omega-3 fatty acids are polyunsaturated fats that are essential nutrients for people. They serve several important functions in the body, such as providing structure to cells and regulating inflammation.
Researchers believe two omega-3 fatty acids, docosahexaenoic and eicosapentaenoic acids, or DHA and EPA, are the most beneficial to overall health. When the body breaks them down, their byproducts have anti-inflammatory effects.
I am a pulmonologist at the University of Virginia School of Medicine, and my research team and I are working to identify risk factors that may contribute to the development of pulmonary fibrosis. In this disease, scarred lung tissue can lead to respiratory failure and death.
We examined whether higher levels of DHA and EPA in the blood of patients with pulmonary fibrosis in different groups of research participants in the U.S. were linked to disease progression. We found that patients with higher levels of omega-3 fatty acids in their blood had a slower decline in lung function and longer survival. Notably, these findings persisted even after we accounted for other factors such as age and co-occurring diseases.
Why it matters
Currently, there are very few treatments available for pulmonary fibrosis. Those that do exist have significant side effects. Our findings suggest that increasing omega-3 fatty acids in a patient’s diet may slow the progression of this devastating disease.
Researchers have investigated the role of nutrition in many other diseases, but it remains understudied in chronic lung diseases, including pulmonary fibrosis. Our study, along with other published research, suggests dietary modifications may influence the trajectory of this disease and improve a patient’s ability to tolerate treatment.
Furthermore, other studies using mice have shed light on how omega-3 fatty acids may protect against pulmonary fibrosis by regulating the activity of inflammatory cells and slowing buildup of scar tissue in the lungs.
What still isn’t known
Since we were able to measure omega-3 fatty acid levels in the blood at only one point in time, we could not determine whether changing levels over time correlates with changes in pulmonary fibrosis.
Crucially, it remains unknown whether increasing omega-3 fatty acid levels in the blood will have a meaningful effect on the lives of patients with pulmonary fibrosis. Omega-3 fatty acids in the blood might not directly affect pulmonary fibrosis and may simply reflect healthier lifestyles and diets.
Clinical trials are necessary to actually determine whether omega-3 fatty acids are beneficial for patients with respiratory diseases.
What’s next
We plan to continue researching whether omega-3 fatty acids have a protective effect against pulmonary fibrosis.
Specifically, we hope to determine the mechanism by which omega-3-enriched interventions affect the lungs of patients with pulmonary fibrosis.
These will be important steps to identify patients who may be particularly responsive to omega-3 therapies and move these treatments toward clinical testing.
John Kim receives funding from the National Institute of Health and Chest Foundation.
Read These Next
Taboo tics like shouting curses and slurs are uncommon in Tourette syndrome − but people who have th
Obscene language tics, called coprolalia, don’t reveal what people with Tourette’s think and feel.…
Why does pain last longer for women? Immune cells may be the culprit
Your immune systems kicks into gear when you’re injured, both worsening and relieving pain.
Honoring Colorado’s Black History requires taking the time to tell stories that make us think twice
This year marks the 150th birthday of Colorado and is a chance to examine the state’s history.