Crisis communication researcher shares 5 key principles that officials should use in coronavirus
Communication from public health and government officials during a health threat is a critical component of preventing and treating a disease. An expert who worked on the anthrax scare explains.

Infectious disease outbreaks have killed more people than hurricanes, wildfires or earthquakes. The 1918 influenza pandemic was the most severe pandemic in recent history, with death estimates ranging as high as 50 million worldwide. Almost 700,000 deaths occurred in the U.S.; in some cases, entire families died.
Because these events are so outside our understanding of what is normal, they create high levels of uncertainty. We don’t know what is happening. And we don’t know what to do to avoid and mitigate the harm.
Crises are also time-sensitive events that require quick decisions and actions to reduce and contain the harm. Delayed evacuations for hurricanes, for example, can lead to more deaths. Failure to issue advisories to boil water can result in disease outbreaks. Telling people what to do during a crisis - boil water, evacuate, shelter in place - is critical to limiting and containing the harm.
I have been studying crises and disasters for over 35 years. Following the 2001 anthrax attacks, I was part of a group of academics that helped the Centers for Disease Control and Prevention develop their crisis and emergency risk communication materials for public health. The anthrax attacks, in which spores of the deadly bacterium were sent through the mail and spread to unwitting recipients, resulted in five deaths. Coming on the heels of the Sept. 11 attack, the anthrax letters caused great fear, and am immediate need for clear communication. I also worked with the World Health Organization to develop guidelines for communicating during emergencies .

Significant research over several decades has developed a body of principles and best practices. The CDC has invested in developing communication resources and competencies for its Crisis and Emergency Risk Communication programs. This evidence-based framework was born out of the 2001 anthrax letters incident and the demonstrated need for effective crisis communication. The framework has informed public health crises for more than a decade. That CDC program and other principles of effective crisis communication share some common features.
1. Credible sources are a must
First and foremost, effective crisis communication is grounded in credible sources .
Dr. John Agwunobi, who was Florida’s Secretary of Health and guided the Department’s 2001 response to letters contaminated with anthrax letters, is an example. His expertise as a public health professional who demonstrated transparency helped manage the public uncertainty. Dr. Agwunobi had no political agenda and made the health and safety of the public his primary concern.
Credibility is a function of trustworthiness and expertise. Trustworthiness concerns the intentions, truthfulness and perceived morality of a source. Expertise reflects the source’s credentials, quality of information and lack of bias. Credibility is necessary for an audience to believe a message and during a crisis, credibility is a critical factor in persuading people to take protective actions.

In the absence of credible sources people turn to alternative sources. Dangerous rumors propagate and go viral. For example, In 2017, rumors circulated widely that Zika virus could be transmitted through casual contact.
Uncertainty, anxiety and stress increase because the public does not believe they are getting the full story. Residents of Hong Kong have lost even more confidence in their government for lack of a transparent and rapid response to COVID-10. Lack of credible sources may enhance the social amplification of risk and can lead to a fundamental misunderstanding of the actual risk the public faces.
2. To reduce rumors, be honest
Effective crisis communication is frequent, honest, and it does not over-reassure. Frequent, honest communication can reduce rumors, needless anxiety and fear, and help quell dangerous rumors. This includes communicating both what is known and unknown about the risk. Irrational anxiety during a crisis is sometimes framed as panic – and used as an excuse for withholding information, offering overly optimistic scenarios, or critiquing or silencing those voices expressing concern. https://www.psandman.com/handouts/AIHA/page13.pdf
The research is clear that panic – extreme, groundless and irrational behavior rarely happens rarely happens during a crisis.
Moreover, the chances of irrational responses to crisis actually are greater in the absence of timely and accurate information. Large, crisis-driven declines in the stock market, for example, are a rational response when there is inadequate credible information about the risks. The antidote to a risk of irrational responses is frequent, credible, transparent and honest communication.
3. Aim for meaningful actions
Effective communication during a crisis involves persuading people to take harm-reducing actions. For example, the CDC has posted guidelines that recommend frequent hand washing and social distancing strategies to help reduce the risk of infectious diseases such as influenza and COVID-19.
Credible information is necessary to promote the kinds of behaviors that can protect people. Effective communication can serve as a kind of social vaccination, encouraging good infectious disease hygiene that reduces harm.
4. Draw from experts, not amateurs
Effective communication during a crisis draws on the knowledge of subject-matter experts. Individuals who have experience and expertise in managing an event are not only more credible, they also have a much better grasp on what actually needs to be done. They are less likely to make fundamental mistakes or misstatements about the nature of the threat and how it might develop. Knowing that the experts are in charge is reassuring to a nervous public.
5. Be consistent
A final factor in effective communication concerns consistency of messages. Messages that offer very different assessments of risk and variable advice about what actions to take increase uncertainty and limit the likelihood the public will take appropriate actions.
Measures such as clearance procedures, whereby messages are reviewed to insure scientific accuracy, can facilitate consistency. Consistency can also be enhanced by having clear and frequent communication from credible sources. Although it is simply impossible to control communication and the flow of information during a crisis, it is possible to influence what is communicated by being credible, honest and frequent.
This responsibility is even more urgent in an era of 24/7 news coverage, multiple social media platforms, and bots and AIs influencing our news feeds. Crises cannot be managed successfully if government and health official do not communicate about them effectively.
[Like what you’ve read? Want more? Sign up for The Conversation’s daily newsletter.]
Matthew Seeger has received funding from the Centers for Disease Control and Prevention, the World Health Organization, the National Science Foundation, and the National Institutes of Health
Read These Next
How a largely forgotten Supreme Court case can help prevent an executive branch takeover of federal
An FBI raid on a Georgia elections facility has sparked concern about Trump administration interference…
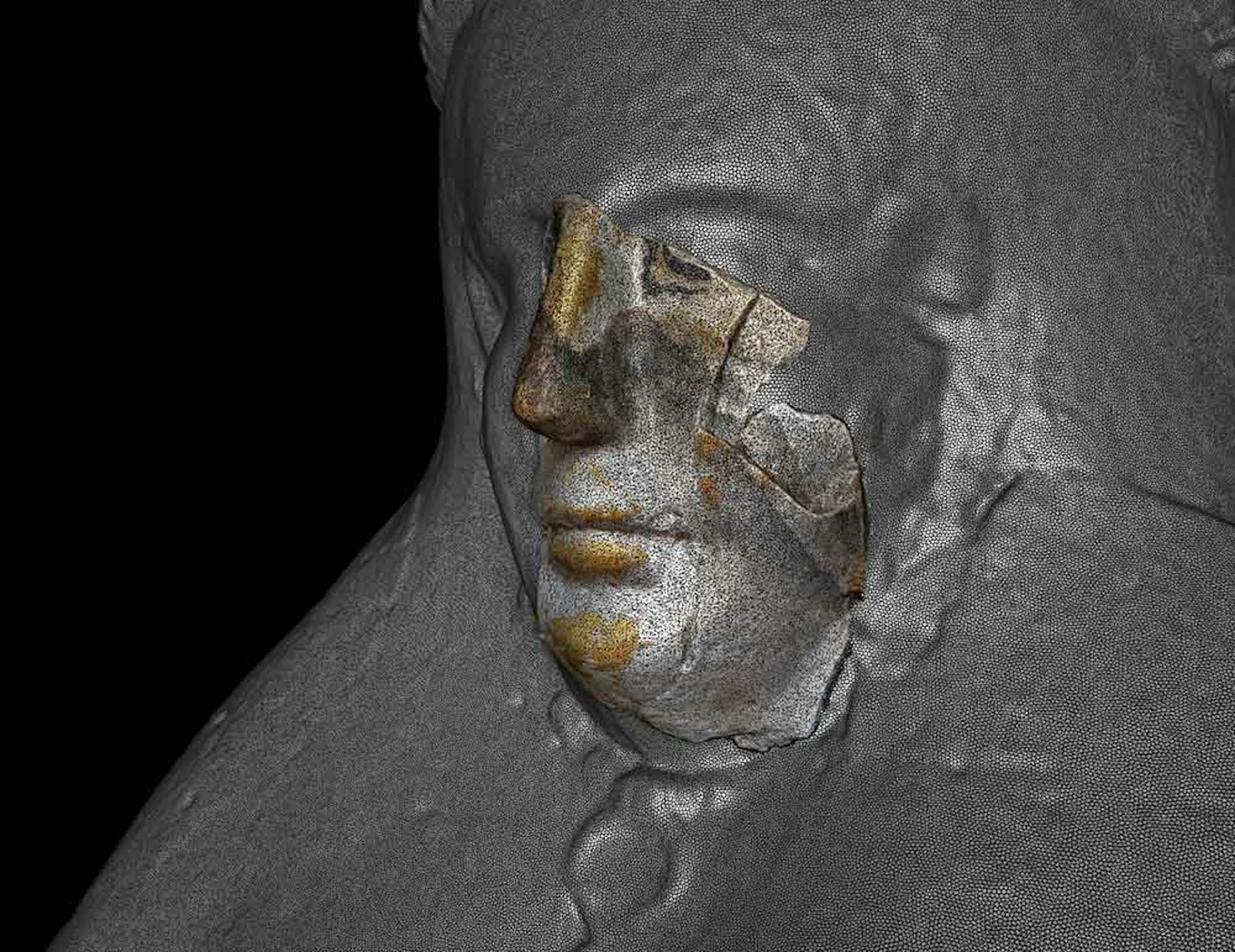
3D scanning and shape analysis help archaeologists connect objects across space and time to recover
Digital tools allow archaeologists to identify similarities between fragments and artifacts and potentially…
Are women board members risk averse or agents of innovation? It’s complicated, new research shows
The effect of women board members on patent activity hinges on whether the company is meeting performance…