Kids exposed to flame retardant PBDE are at risk for lifelong liver or cardiovascular problems
Brief exposure to a family of chemicals used as flame retardants early in life can permanently alter fat levels in the blood and liver, raising the risk of liver cancer and heart disease.

What factors determine if you will experience healthy and cheerful aging or if it will turn into an endless chain of suffering from numerous health conditions?
Many factors shape our health, including genetics, diet, physical activity, smoking and stress. Some other factors may be as powerful but may not yet be recognized.
I am an environmental toxicologist studying how man-made chemicals affect our health. I was always interested in understanding how our current health is shaped by chemical exposures during the embryonic and early postnatal period – life stages that are particularly sensitive to environmental stressors.
To address these questions, I focused on the analysis of long-term health effects induced by a family of chemicals used as flame retardants called polybrominated diphenyl ethers (PBDEs). The first patent for PBDE use as a flame retardant was issued in 1960, and manufacturing of commercial products containing PBDEs, such as building materials, electronics, furnishings, motor vehicles, plastics, polyurethane foams, baby pajamas and others, began in 1965. PBDEs were first detected by scientists in animal tissues in the 1980s.
Later studies showed that concentrations of these chemicals in human blood, milk and tissues were increasing exponentially over the past 30 years, doubling every five years, while their health effects were poorly understood.
Early exposures trigger lifelong changes in blood lipids
In one of my experiments, I fed mice one of the PBDEs most often found in human blood and milk – BDE-47. The female mice received it from day 8 of their pregnancy until the end of nursing (postpartum day 21).
We exposed mice to 0.2 milligrams of this chemical per kilogram of body weight. This caused BDE-47 concentrations in the fat of experimental animals to reach similar levels to concentrations found in humans living in big American cities. This comparison is used in toxicology to ensure that laboratory experiments use doses relevant for human exposures.
We were surprised to find that triglyceride levels were significantly altered in the offspring of exposed mothers, even though exposure to BDE-47 ceased three months earlier. Triglycerides are main constituents of body fat and cell membranes in humans and other animals.
To understand how BDE-47 changes blood triglycerides and other lipids, my laboratory conducted another experiment with mice. Lipids are insoluble molecules that are used to store energy and as structural components of cell membranes.
We hypothesized that changes in blood lipids result from changes in liver function. It is well-known that the liver regulates composition of lipids in blood. The liver can synthesize new lipids, destroy them, secrete lipids to blood and absorb them from blood.
To test our hypothesis, we exposed female mice to BDE-47 daily during pregnancy or during the period of lactation and analyzed health outcomes in offspring when they reached one year old – roughly equivalent to 50 years in humans.
This experiment again demonstrated that short-term exposure to BDE-47 during early steps of development results in long-lasting effects on blood lipids in mice. These effects were very similar in animals that were exposed during the embryonic period or during nursing.
Reprogramming the balance of lipid in blood and liver
In exposed animals, levels of blood triglycerides fell by half, and livers accumulated 20 percent to 40 percent more lipids than in mice that were never exposed to the chemical. Activity of many liver genes encoding enzymes important for lipid metabolism was altered in exposed mice.
Among key proteins involved in lipid metabolism, one was particularly high. This protein – CD36 – is responsible for pumping lipids from blood to the liver. Increased amount of CD36 in exposed animals is likely responsible for lowering lipids in blood and raising them in the liver, resulting in increased accumulation of these fats in the liver.
We observed that lower-exposure dose (0.2 mg/kg) and higher-exposure dose (1.0 mg/kg) regulated CD36 in opposite directions. Lower dose resulted in decreased CD36 and elevated blood triglycerides, while higher dose raised CD36 and decreased blood triglycerides. We think it is important to note that both tested doses were in the range of human exposures.
Do changes in CD36 pose health risks?
Our findings demonstrate that exposure to BDE-47 during early development can alter the levels of CD36 in either direction in mice and that both increase and decrease in CD36 may be deleterious.
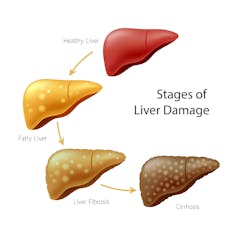
When we exposed mice to high doses of BDE-47, this increased levels of the CD36 protein, which causes excessive accumulation of fat in liver cells. This condition is called nonalcoholic fatty liver disease. It is the most common form of chronic liver disease among adults and children.
Around one-third of the American population has nonalcoholic fatty liver disease, and it is a risk factor for Type 2 diabetes, hypertension, cardiovascular and kidney disease, liver cirrhosis and liver cancer.
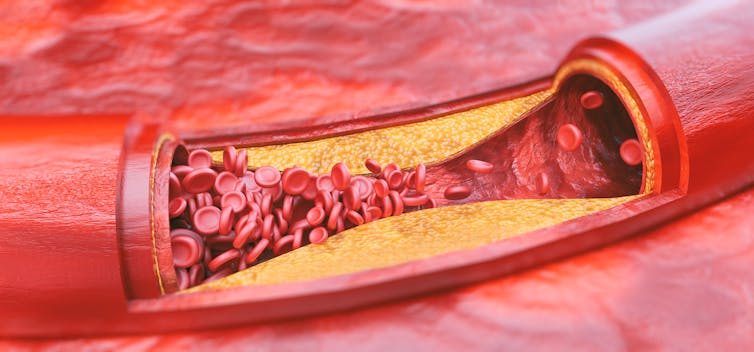
On the other hand, decreased activity of CD36 will lead to higher lipid levels in the blood and result in atherosclerosis – a disease in which plaques of lipids build on the walls of vessels. Atherosclerosis is the primary risk factors for heart attack, which causes around 800,000 deaths annually in the U.S. alone. Thus, early life exposure to this environmental chemical may completely reprogram lifelong health trajectory.
Studies published by other laboratories confirm that PBDEs disrupt lipid metabolism in rats and increase risk of nonalcoholic fatty liver disease in mice exposed during early steps of development.
Still at risk?
PBDEs were banned in Europe by 2008 and voluntarily withdrawn by industry in North America by 2013. It is likely that PBDEs’ production ceased all over the world, although data are missing for many regions. However these chemicals are still present in products used in U.S. households and cars. PBDEs are very stable compounds. Once released into the environment, they accumulate in sediments and in fatty tissues of wildlife and humans and stay there for many years. For example, the half-life of different PBDEs in the human body is between one and seven years. In the environment they found their way to fatty tissues of animals, many of which represent important sources of food for us.
Although production of PBDEs has ceased in developed countries, some studies report that concentrations of PBDEs in human tissues in the U.S. continue to grow.
People born in the U.S. and Canada during the last 15 to 20 years were exposed during their early life to environmental concentrations of PBDE, comparable to those that reprogrammed lipid metabolism in our experiments with mice. Thus, we believe that about 20 percent of the North American population may be at risk of conditions associated with altered lipid concentrations in blood and liver.
Will these people develop aging-related conditions more readily than previous generations? The answer is yet to come. It is likely that PBDEs are not the only culprit. Many other ubiquitous pollutants, such as polychlorinated biphenyls (PCBs), dioxin (TCDD) and perfluorinated compounds (PFOS, PFNA), are known today to affect CD36 in mice.
It is not yet clear if effects of these other chemicals are as long-lasting as effects of PBDE. It is also not yet clear if effects of chemical exposures observed in mice are the same in humans. Mice are the most widely used animal model for testing the toxicity of pharmaceuticals and industrial chemicals, and animal toxicology studies generally are applicable to humans, although responses of laboratory animals and humans to chemicals may differ in type and severity.
Alexander Suvorov receives funding from: 1. University of Massachusetts - Amherst (startup funding), expired 2. Institute of general Genetics of the Russian Academy of Sciences (research contract), expired 3. USA Department of State (research grant), expired 4. USA National Institutes of Health (research grant), current
Read These Next
GLP-1 drugs may fight addiction across every major substance, according to a study of 600,000 people
GLP-1 drugs are the first medication to show promise for treating addiction to a wide range of substances.
Housing First helps people find permanent homes in Detroit − but HUD plans to divert funds to short-
Detroit’s homelessness response system could lose millions of dollars in federal funding for permanent…
I study why zebrafish larva prefer to circle left or right, to understand how and why human brains e
Being left- or right-handed – and the paw, eye, fin and wing equivalents – is a product of genes,…