Dying while black: Perpetual gaps exist in health care for African-Americans
Gaps in care and outcomes between African-Americans and white patients is a major concern to those who care about fairness in health care. Gaps in care also exist at end of life, too.

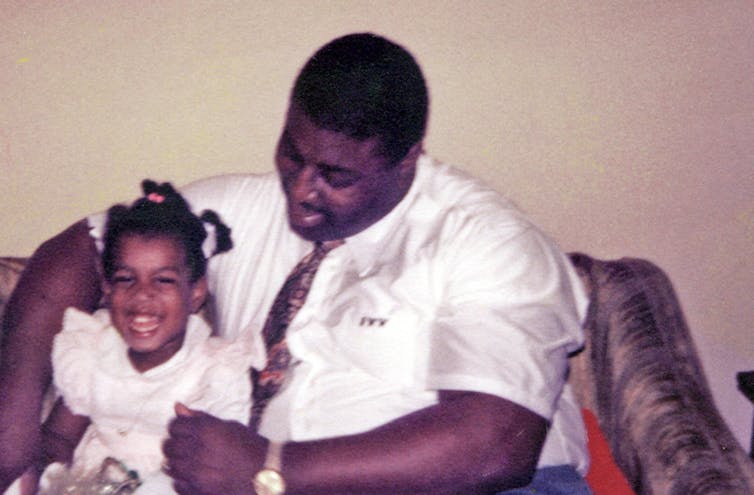
Several years ago, MapQuest directed me on a 10-hour drive to visit my father in a Florida hospital. Complications from diabetes, including blindness, kidney failure, congestive heart failure, and a below-the-knee amputation, had taken their toll. This time my father, 69, was hospitalized for an infection of unknown origin that physicians could not name, despite their many attempts to grow cultures.
I did not know it at the time, but my father was dying.
Once I arrived at the hospital from Durham, North Carolina, I could hear his screams from the nurses’ station. “Never mind. I hear him,” I told the nurse whom I had just asked the location of my father’s room. “I’ll follow the sounds.”
That any patient would be left in so much pain that his screams could be heard down the hall was unacceptable to me. That this patient was my father, a man I had always known as a big, strong former football player – the kind of man other men didn’t dare cross (but who was also loving and gentle) – was difficult for me to process. Yet, here I was, being guided to his hospital room by the sound of his cries. Despite being a trained philosopher with an interest in bioethics, I had not yet begun to think about the ways in which racialized health disparities manifest even at the end of life. My father’s excruciatingly painful process of dying was but one example.
Gaps while living, gaps while dying
It is well documented that African-Americans experience excess mortality, or deaths beyond the expected mortality rate. However, even if disparities in the mortality rate for African-Americans were rectified tomorrow, the fact remains that we will all eventually die. And how we die matters.
According to a 2013 Pew Research survey, 72 percent of American adults have given at least some thought to their end of life wishes, with 37 percent of American adults having given their end of life wishes a “great deal of thought.” Some of these wishes include decisions about pain management, maintaining quality of life, and whether to continue aggressive medical treatment for terminal illness.
Additionally, research shows that people tasked with making treatment decisions for loved ones who cannot express their own wishes sometimes experience distress about watching their loved one suffer. Even months or years later, they wonder whether they made the “right” decision.
Pain ignored
Black patients generally receive worse pain management in primary care environments and emergency rooms. Even black children are not treated for their pain to the extent that white children are. Some attribute this to false beliefs about biological differences between black and white patients, including the belief that black people have “thicker skin” and, therefore, do not experience as much pain as whites. These false beliefs lead to inaccurate pain assessments by physicians evaluating black patients and an unwillingness to take the pain complaints of black patients as seriously.
This disparity in black patients’ pain management continues even as black patients are dying. Families often want to ensure that their loved ones are as comfortable as possible once patients reach the point where death is near. Racialized gaps in pain management lead to a denial of humane comfort care that contributes to unnecessary suffering for black patients and their loved ones.
Symptoms ignored

Inadequate pain management is but one aspect of the lower quality of care that black patients report in general that affects when and how black patients die. In December 2015, 57 year-old Barbara Dawson was arrested and forcibly removed from Calhoun Liberty Hospital near Tallahassee, Florida, after she refused to leave without further treatment. Although she had been evaluated in the hospital, she was discharged despite her continued complaints of difficulty breathing. Hospital personnel apparently assumed she was faking her symptoms and called police to arrest her for being disruptive. Dawson collapsed before she could be placed in the police cruiser and was returned to the hospital where she died an hour later from an undetected blood clot in her lungs.
Dawson may or may not have been at the end of life when she arrived at the hospital. However, hospital staff allowed her condition to deteriorate by not taking her complaints seriously. She died only feet away from people who could have, at minimum, eased her process of dying. The hospital was later fined US$45,000, and Dawson’s estate settled a lawsuit against the hospital for $200,000 in 2017.
Less interaction
Dawson’s experience is a dramatic and appalling case. Nevertheless, one groundbreaking study revealed that physicians generally interact less – both verbally and nonverbally – with black patients who are dying than with white patients who are dying. At the end of their lives, black patients do not receive the same comfort care, including eye contact and touch, from physicians that white patients do.
The U.S. health care system can improve care for all patients at the end of life. However, this system still denies black patients the kinds of interventions that white patients often take for granted. This denial contributes to more painful, horrific deaths of black patients and compounds the grief of their loved ones.
In my father’s case, even as part of me still hoped for a miracle, the thing I wanted most in the world was for him to be as comfortable as possible. That this did not happen despite my best efforts still haunts me when I think about the end of my father’s life.
Yolonda Wilson does not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Read These Next
Why Stephen Colbert is right about the ‘equal time’ rule, despite warnings from the FCC
The ‘equal time’ rule has been around for a century and aims to promote broadcasters’ editorial…
Supreme Court rules against Trump’s emergency tariffs – but leaves key questions unanswered
The ruling strikes down most of the Trump administration’s current tariffs, with more limited options…
After a 32-hour shift in Pittsburgh, I realized EMTs should be napping on the job
A paramedic and university professor shares data about how strategic napping could help his own health…