Drug development is no longer just for Big Pharma. Researchers at Bio-X explain
Developing drugs is typically the domain of large pharmaceutical companies. But here is an example of drug development for a rare pediatric brain cancer that was done in a university setting.

I am a graduate student and resident in the field of neurosurgery and would like to share an unusual and very personal story of developing a drug. Developmental biologist Dr. Matthew Scott and I went from purely basic biological research in our lab at Stanford University to discovering a target for drug development to identifying a drug for a pediatric brain cancer called medulloblastoma to a clinical trial – all within five years and for just US$500,000, with the money raised through philanthropic donations.
That’s surprising for two reasons. First, the odds of successfully getting a drug to clinic are very low. For every 10,000 candidate drugs, only five are ever tested in clinical trials. The few that do make it into pharmacies have on average a $1 billion development cost for research, testing and clinical trials. For this reason, the gap between scientific discoveries and clinical trials is commonly referred to as the “valley of death.” The other reason my experience is atypical is because most new drugs are developed for a disease of interest by pharmaceutical companies. In contrast, we identified existing drugs that were developed for other diseases, but could be repurposed.
Our basic science approach shaved a decade off the usual development time. The clinical trial will begin this winter, so whether we succeed remains to be seen. But our story is worth sharing as a promising path for finding new drug candidates.
A rare childhood cancer in need of treatment
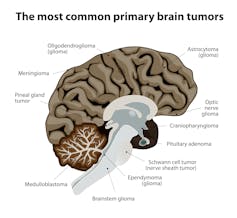
A very specific disease led me to drug development. Medulloblastoma is the most common pediatric brain tumor. Brain cancer is the leading cause of cancer-related death in children. Children with medulloblastoma undergo surgery, then whole brain radiation, and finally chemotherapy. Even kids who survive the disease are often burdened with severe therapy-related problems – such as intellectual and social impairment, endocrine dysfunction, hearing loss and secondary, treatment-related cancers – that harm their long-term quality of life.
Medulloblastoma, intractable in the past, was primed for discovery of transformative therapies by new scientific discoveries. Research advances revealed that genetic damage to a single signaling system in cerebellum cells, called the hedgehog signaling pathway, caused a third of all medulloblastomas. The hedgehog pathway has been a good target for drugs.
The underlying biology is unusually straightforward. Hedgehog signaling during normal brain growth stimulates the proliferation of cerebellum cells. When no more signal is made, soon after birth, the cerebellum growth stops. A genetic mutation or chemical that activates hedgehog signaling at later times leads to uncontrolled growth of the cerebellum and eventually medulloblastoma. My goal was clear – to be able to shut down hedgehog signaling and stop the growth of this cancer.
Discovering a new drug target
The first step was finding a lab with a history of important discoveries in the hedgehog signaling pathway and a mentor interested in translating basic discoveries into medicine. Matthew Scott was that mentor. His team had linked hedgehog signaling to cerebellar development and medulloblastoma.
To discover a better therapy, we focused on identifying proteins that control normal growth of the cerebellum. We hoped this would provide clues about signals controlling the growth of tumors.
We used advanced techniques to look at modifications of thousands of proteins, particularly those altered by hedgehog signaling. We identified an enzyme called protein kinase CK2 that causes normal cells to divide in the developing cerebellum by activating hedgehog signaling. Medulloblastomas are derived from cerebellum cells, and like normal cerebellum cells are dependent on hedgehog signaling for growth. We inferred that CK2 might also be required for growth of the tumor cells.
Using mouse tumors and human tumor cells, we tested drugs shown to be safe in humans and discovered ones that blocked CK2, and killed off medulloblastoma cells. The drugs were effective even against the most aggressive forms of human and mouse medulloblastoma that are resistant to current therapies. Half the mice with medulloblastomas treated with CK2 blockers survived for over a year. Mice receiving the placebo died within 17 days of tumor growth.
After we discovered how well CK2 drugs blocked medulloblastoma tumor progression, our group partnered with Stanford SPARK, an academic drug development program; Senhwa Biosciences, a biotechnology company that owns the only human-tested CK2 inhibitor; and the Pediatric Brain Tumor Consortium (PBTC), an NIH-funded group of 12 pediatric hospitals dedicated to clinical trials for brain tumors in children. A clinical trial to test CK2 inhibitors for children with medulloblastoma is planned for this winter. It is expected to run for three years.
Smart architecture fosters collaboration

Close to 95 percent of new drugs are developed by large drug companies. Drug development doesn’t typically happen in academia, and even when it does it is usually not done by a basic science researcher.
Large drug companies focus on common, more lucrative diseases like high blood pressure, high cholesterol, and conditions like pain management that affect tens of millions in the U.S. alone, for example. By some accounts, it costs, on average $1 billion to get a drug to market. Drug companies recover their investments when there are large markets for their drugs, such as with statins. The US Preventative Services Task Force suggests that more than 17 million people would be good candidates for these drugs. The promise of profits is small with less common diseases. Could it be that developing new therapies for less common diseases, such as childhood brain cancer, may best be done by partnerships involving academic scientists?
This project began during a serendipitous encounter between members of the Scott lab, which studies how genes control animal development, and the Elias lab, which specializes in a technique that allows scientists to detect changes in proteins. Both of these labs were located in the Clark Center – the home of Stanford Bio-X, a program and building designed to promote interdisciplinary research and encourage cross-pollination.
Students must walk through other labs to get to stairways and exits. Desks and benches from different labs are intermixed. Large instruments, core facilities, and the coffee bar and restaurant areas are shared to encourage intermingling. Within the building are faculty from more than 25 Stanford departments.
Shared success provides rich rewards

What happened in our work with SPARK could in principle happen at biomedical centers all across the country, but several convergent factors were required for success.
First, we were lucky that the technology licensing office at Stanford connected our project to SPARK, which in turn connected our academic team with startup CEOs, seasoned pharmaceutical executives and patient advocates. Without this string of strategic connections, we would not have had the know-how to take the project beyond the bench, nor the credibility to convince Senhwa to sponsor the trial.
Second, our research was supported by philanthropists and was driven by scientists and clinicians who are not financially invested in the success of the project. Therefore, creating profitability from a therapy developed for a rare disease, which is a major barrier for pharmaceutical companies, was not a problem we had to tackle. This allowed us to repurpose someone else’s drug, which dramatically reduced the time and cost required to bring a therapy to patients.
Finally, our collaboration with Senhwa was solidified by the PBTC, the nonprofit consortium created by the National Cancer Institute to improve treatment of primary brain tumors in children. Without federally funded, multi-institutional collaborations, like the PBTC, the cost and expertise required for designing and implementing trials for children with brain cancer would have been well out of our reach.
In medicine, you experience tremendous fulfillment when you provide hope, and when you alleviate the fear and suffering of others. In drug development, you grind through countless biological, political and financial barriers and hope to come out having transformed an idea into an actual physical product that may change how we treat disease.
Our experience has provided a rich sense of excitement and potential for improved patient survival and recovery. In contrast to the stories of combative and avaricious high-stakes science and drug development we sometimes hear, our success can be attributed to a diverse team of international collaborators who donated their time and energy to support a common goal – providing better options for children with brain cancer.
Teresa Purzner receives funding from the Felix and Heather Baker BioX Stanford Interdisciplinary Graduate Fellowship, the Neurosurgery Research and Education Foundation Foundation (NREF), Stanford SPARK, the Department of Developmental Biology, Stanford School of Medicine, the Weston Havens Foundation and NIH grant R21HD076367
Read These Next
As war in Ukraine enters a 5th year, will the ‘Putin consensus’ among Russians hold?
Polling in Russia suggests strong support for President Vladimir Putin. Yet below the surface, popular…
After a 32-hour shift in Pittsburgh, I realized EMTs should be napping on the job
A paramedic and university professor shares data about how strategic napping could help his own health…
How Dracula became a red-hot lover
Count Dracula was originally a rank-breathed predator. His transformation into a tragic romantic mirrors…






