Think teens need the sex talk? Older adults may need it even more
Studies confirm what many older adults already know: They are sexual. And, studies also suggest that sex is good for them.. So why do health care providers not want to have a sex talk with them?

Humans are sexual beings. This urge does not stop when the clock strikes 60. Or even 90.
Young adults may deny older relatives are having sex, but sexual activity is a strong indicator of healthy aging and vitality. In fact, sexual activity is roughly equal to climbing two flights of stairs.
Sex education and research use a medical model of sexual health focusing mainly on pregnancy, sexually transmitted infections (STIs), and sexual dysfunctions. However, sexuality is complex. Beyond genitals and Kama Sutra-like positions, it considers sexual and gender identity; sensuality; sexual response; intimacy; and positive and negative ways we use our sexuality.
Our research has explored sexuality among older adults experiencing healthy aging and also aging with health challenges. We found that older adults who routinely talk with health care providers about sexual matters are more likely to be sexually active, despite sexual dysfunctions or other health issues. These conversations become more important considering high HIV/AIDS and STI rates, even among older adults in the U.S.
Sexuality is complex
As we age, the complex interplay among biological, psychological, cognitive, socioeconomic, religious and even societal factors, contribute to changes in our roles and responsibilities. For example, changes in physical or cognitive health over time can create differences in analytical thinking, mobility, and health care needs. We also experience changes in work, social and family roles and responsibilities over time. Examples include transitions from working to retirement, parenting to empty-nesting, child-rearing to caring for aging parents or partners.
These changes may alter our sexual desires, expression and the frequency in which we engage in sexual activities with partners. For example, sexual functioning and activity may decrease over time, but having open communication with a partner who is responsive to our needs can increase our feelings of intimacy and desire, and in turn stimulate sexual activity.
Evolving social support and activities may change opportunities for sex and intimacy. Partners may disappear through death or moving away, or appear, such as when meeting new people after moving to an aging community. Over one-third of adults over age 65 use social media or internet technologies. These tools may expand sexual interest or activities by increasing access to sexual aids and partners.
Sex after 60

There are myths, misconceptions and stigma associated with aging and sexuality that hinder older adults’ ability to openly communicate with family, friends and health care professionals. This misinformation limits their access to sexual education, health care, and ultimately, their sexual rights.
The first myth is that older adults are not as sexually attractive or desirable as their younger counterparts. While an 80-year-old may not be as appealing to an 18-year-old, he or she may be very desirable to peers. More importantly, he or she may feel more sexually desirable and confident than their younger self.
A second myth is that older adults lack interest in and desire for sexual activity – and that they are somehow asexual. Research from ongoing national surveys support the ideas that sexual interest, desires and behaviors can decrease over the life course. For example, among women ages 57 years and older, over 80 percent of participants expressed interest in having sex, but less than two-thirds of women surveyed perceived sex as “important,” and fewer than half reported having sex in the previous year. However, the reality is that these trends are not universal among older adults. Results from another recent survey found that 39 percent of men and 17 percent of women ages 75 to 85 years are sexually active.
Another myth is that older adults are so medically fragile that sexual activity is dangerous. This is simply not true in many cases. Recent studies have shown that healthy older adults are more likely to have sex. Even when chronic illnesses are present, sexual abstinence is not a foregone conclusion. For example, a 2012 American Heart Association statement contains evidence-based recommendations about sexual activity among patients with specific cardiovascular conditions. The recommendations generally advise assessing risks with a doctor and disease management, rather than abstention.
There are well-documented relationships between common medical conditions such as heart disease or diabetes and treatment-related effects on sexual functioning. Yet, older adults and their health care providers are not discussing sexual concerns during routine care. Missed opportunities during visits deprive older adults of access to newer treatments and other best practices in sexual medicine, which can impact their mental and physical health.
A bigger problem may be ageist attitudes among providers and internalized ageism in their patients that may interfere with sex education and application of newer standards. The result is that many believe older adults are uninterested in, or lack desire for, sexual activity and cannot engage in these activities.
Love has a lot to do with it

There is more to sexuality than physical acts. While much of the existing research focuses on sexual activity and intercourse as predictors or outcomes, most older adults also desire companionship, intimacy and closeness. Non-intercourse-focused activities, such as hand-holding, cuddling and massage, have not been studied as much as intercourse. Yet, there is reason to believe that they can enhance intimacy. Research about physical and mental health outcomes resulting from older adult sexual activity reveals additional benefits, including reduced cognitive decline, loneliness and depression, and improved reported health status, physical functioning, and other aspects of quality of life.
Recent studies also reveal that sexually active older adults are more likely to communicate needs and concerns with health care providers and have them addressed. Providing high-quality sexual health care requires providers to take comprehensive sexual health histories from older patients and engage in direct, positive communication concerning gender and sexual identity, and sexual knowledge, beliefs and practices.
Discussions should promote understanding about sexual risk behaviors for STIs and effects of physical and cognitive or psychological aging on sexual health and sexuality. To maintain or improve older adults’ sexual health and well-being, health care providers should provide safe and welcoming environments for patient-provider collaboration, resources and interdisciplinary referrals to clinical social workers, sex therapists, physical therapists and other allied health specialties.
The authors do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
Read These Next
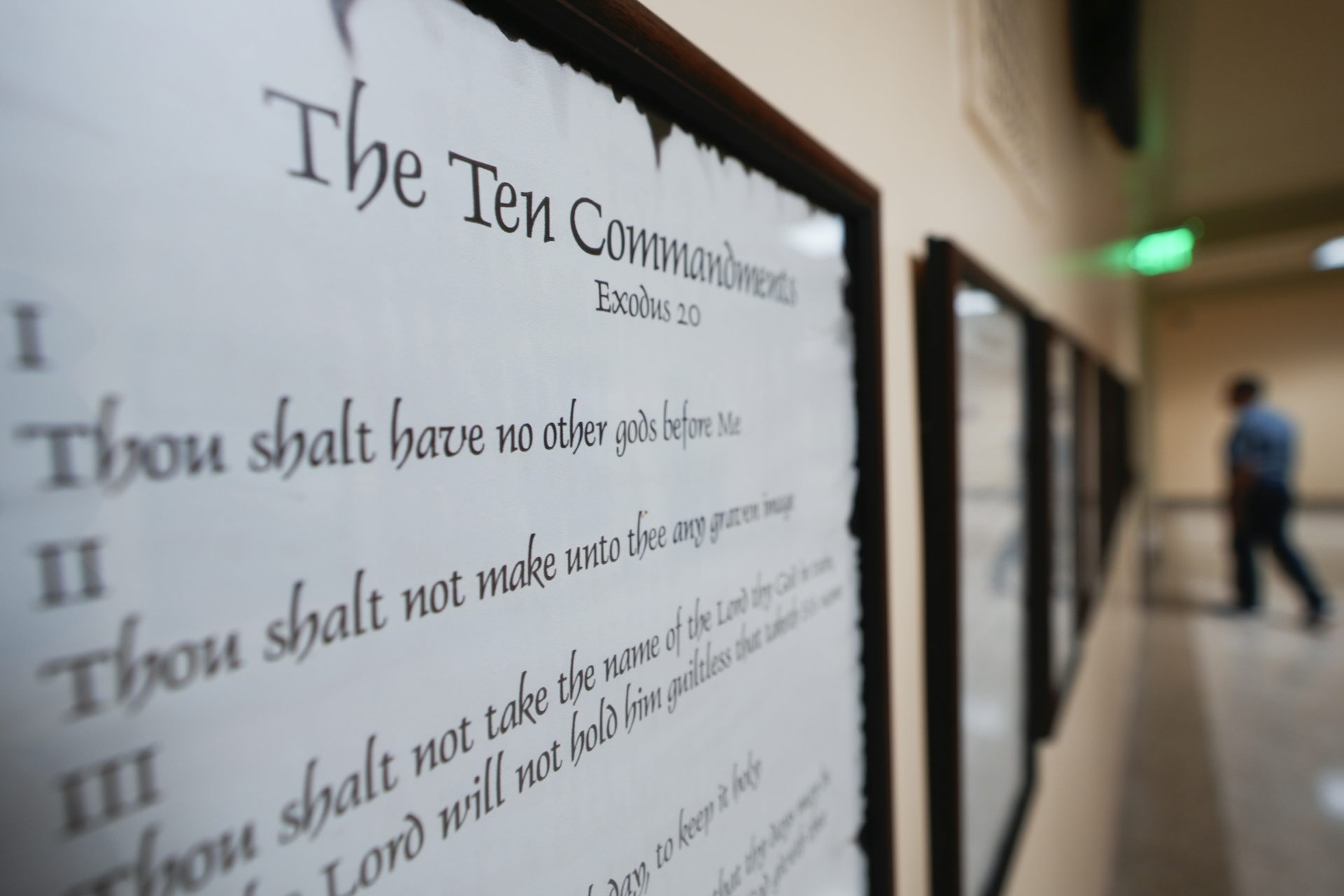
Baptists have helped shape debate about religious freedom for over 400 years – up to today’s 10 Comm
The phrase ‘separation of church and state’ dates back to a letter from Thomas Jefferson to a Baptist…
What is Bluetooth and how does it work?
Did you know that your wireless earbuds contain a tiny radio transmitter?
Meekness isn’t weakness – once considered positive, it’s one of the ‘undersung virtues’ that deserve
The word ‘meekness’ might seem old-fashioned – and not a positive trait. But understanding its…