Accelerating health care innovation by connecting engineering and medicine
Health care relies on increasingly sophisticated devices for implanting into the body or monitoring it. Yet most med school graduates are not versed in engineering. That needs to change.
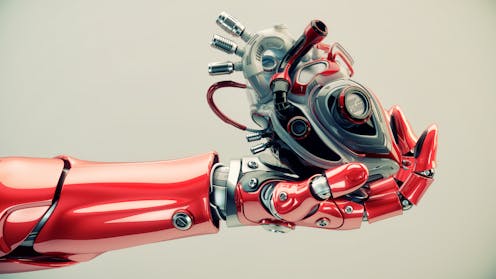
Artificial heart valves, prosthetic hips, bedside monitors, MRI machines – these and so many other innovations that we now take for granted emerged at the interface of engineering and medicine.
In an era of big data, personalized medicine and artificial intelligence, the importance of engineering, especially in medicine, is increasing. In my own field of cardiovascular bioengineering, engineers now routinely build and run sophisticated, patient-specific computer models of blood flow in just a few hours, helping doctors diagnose and treat heart disease. These groundbreaking inventions are possible only through the contributions of multidisciplinary teams of researchers, clinicians and engineers.
The rise of biomedical engineering

Engineering schools are preparing for this future in part through the growth of biomedical engineering, where students learn not only the tools and concepts of engineering but also how to apply those ideas to today’s medical challenges. Many aspects of modern healthcare – from designing implants that survive for decades in the body to constructing secure medical records systems – are driving the demand for biomedical engineers.
In 1974 only three engineering schools offered accredited biomedical engineering programs. Forty years later, in 2014, more than 100 accredited programs granted bachelor of science degrees in biomedical engineering or bioengineering. In line with broader trends in engineering education, these programs prepare students to collaborate by challenging them with team-based projects.
As a result, our nation’s young biomedical engineers have the engineering expertise, appreciation for collaboration and at least some of the medical vocabulary they need to communicate effectively with physicians.
A gap in medical training
Yet, nothing in my medical school curriculum was designed to help physicians develop a complementary skill set. Every physician now uses advanced technology during the course of their daily work. But only a handful have the technical vocabulary or training required to help develop it. Several medical schools have recognized the need for engineering-literate physicians, building new campuses and launching new programs that blend medical and engineering education. Yet, many of these efforts are employing an outdated, physician-centric model that envisions training one person in two disciplines, rather than preparing them to collaborate in multidisciplinary teams.
This one-person, two-discipline approach has a long history at medical schools, exemplified by prestigious M.D.-Ph.D. programs that seek to train physician-scientists who split their time between caring for patients and conducting research.
While these M.D.-Ph.D. programs have been successful in some respects, they train only a small number of doctors. As recently reported by the American Association of Medical Colleges (AAMC), M.D. and Ph.D. programs are producing approximately 600 graduates per year, a number that is limited in part by financial resources; these students represent only 3 percent of medical school graduates but receive 17 percent of non-need based medical school scholarships. Joint programs that incorporate graduate engineering degrees will be further limited by the pool of applicants qualified for both medical and graduate engineering study.
Collaboration: A proven, scalable approach

That is why we need a new approach: a proven, scalable approach at the engineering-medicine interface that teaches engineers and health care professionals to work together in teams.
At the University of Virginia, our Center for Engineering in Medicine promotes innovation by embedding engineering students into clinical environments and nursing and medical trainees into engineering laboratories. Embedded students acquire the technical vocabulary, cultural literacy and experience working in multidisciplinary teams that provide a foundation for careers in health care innovation.
Teaching engineers and health care professionals to collaborate is faster, cheaper, and more feasible than building specialty programs to train physician-engineers or launching more biomedical engineering programs. Teaching engineers and healthcare professionals to collaborate is faster, cheaper, and more feasible than building specialty programs to train physician-engineers or launching more biomedical engineering programs. This approach builds on the experience of successful programs like Stanford Biodesign and the Coulter Translational Partners Program, and is especially attractive at institutions like UVA, where engineering and medical schools are located on the same campus.
Overcoming distance
However, many universities in America are not built to promote collaboration between the fields of engineering and medicine. In part, that is because schools devoted to agriculture and engineering are often miles from those focused on liberal arts and medicine. In situations where physical proximity is not possible, workshops, conferences, continuing medical education courses and cross-disciplinary events can spark the cross talk that catalyzes innovation.
Finding ways to reduce literal, and disciplinary, separation between engineering and medicine is essential for cultivating and expanding innovation at the interface. While new specialized training programs may play a role in this effort, promoting collaboration within the existing workforce has the potential to make a much bigger impact.
The leaders in the next wave of health care innovation will be the universities, health systems, and companies that find ways to train engineers, doctors, nurses and others to work together effectively in teams to solve tomorrow’s complex health care challenges.
Jeffrey W. Holmes has received research grants from the National Institutes of Health, the National Science Foundation, the American Heart Association, and the Paul G. Allen Frontiers Group. He trained in a joint MD/PhD program with scholarship support from the National Institutes of Health.
Read These Next
China’s muted response over war in Iran reflects Beijing’s delicate calculus as a concerned onlooker
Beijing has denounced US-Israeli action in Iran, but has not rushed to come to the aid of its regional…
How Instagram addictiveness lawsuit could reshape social media – platform design meets product liabi
A lawsuit against Meta and Google avoids the issue of liability for content and focuses on allegations…
Family-friendly workplaces are great − but ‘families of 1’ get ignored
In an era of family-friendly workplaces, how can employers treat single people without kids fairly?




