Prenatal blood screening may predict Zika virus-associated fetal defects
There is no vaccine or medicine for Zika. But researchers have identified factors in the blood that signal a fetus has Zika-related birth defects, helping mothers decide whether to terminate a pregnancy.
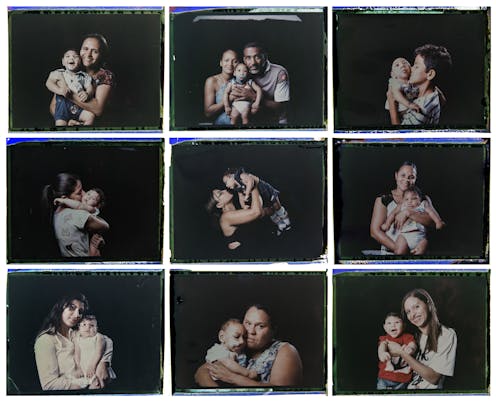
The sudden and rampant outbreak of Zika virus in 2016 terrified pregnant women, particularly those residing in Zika-endemic regions, such as Brazil, as well as those in the U.S. Their fear was justified given the link between Zika virus infection during pregnancy with having a small head, a condition known as microcephaly, and other congenital defects.
The absence of early prenatal diagnosis, or treatment, for birth defects has left thousands of mothers-to-be worrying about their baby’s well-being. Others, meanwhile, have terminated their pregnancy rather than risk having a child with birth defects.
Our research revolves around mosquito-borne viruses such as Chikungunya virus and Zika virus. Each causes a distinct set of symptoms. Chikungunya virus produces debilitating persistent joint pain in adults and neurological symptoms in children; Zika virus causes defects in babies. In Jae Jung’s lab at the University of Southern California, we are investigating the mechanisms that underlie the devastating consequences of these viral infections and developing new prenatal diagnostic tests to determine whether Zika babies are in good health.

Zika and pregnancy
Zika is the first mosquito-borne virus known to cause congenital defects. Aedes aegypti, one of the most invasive and widespread species of mosquito, is the primary vector for transmitting Zika. When healthy individuals, who are not pregnant, are infected with the Zika virus the infection often escapes notice because the symptoms are mild or negligible. However, infection during the first and second trimester of pregnancy boosts the risk of miscarriages and diverse fetal defects such as eye abnormalities, neurological impairment and in more severe cases, microcephaly.
Health workers try to assess the health of Zika babies using ultrasound during the second trimester or later. But it is difficult to see from these images whether the baby has developmental abnormalities.
On the other hand, fetal MRI captures high-resolution snapshots of the fetus. But this imaging technique can only be used in the second or third trimesters – when it is more difficult to terminate a pregnancy. A diagnostic assay that could detect abnormalities early in the pregnancy could alleviate the mother’s stress and make it easier to make swift reproductive decisions.
Developing a new diagnostic test
During the Zika outbreak in Brazil, there were other co-circulating mosquito-borne viruses such as Dengue virus and Chikungunya virus. So we also chose to take blood samples from women from the U.S. where these viruses are not endemic. In our recent research, we surveyed blood samples from 74 pregnant women: 30 were Zika-positive, 30 were negative and 14 were from women in Los Angeles. This study was led by Jae Jung, in collaboration with Patrícia Brasil of the Instituto Nacional de Infectologia Evandro Chagas in Brazil, and Karin Nielsen-Saines and Genhong Cheng of UCLA.

Our findings revealed an elevated production of 16 specific protein biomarkers, which are present in the blood of pregnant women who gave birth to babies with developmental delays and eye abnormalities. These biomarkers are potentially useful for predicting the outcomes of Zika pregnancies simply using blood specimens from the mother-to-be at any stage of pregnancy.
The number of Zika cases has dramatically declined following the major outbreaks in 2016. Yet, many Zika babies are still suffering from the dire consequences of prenatal infection. With the widespread abundance of Aedes mosquitoes, and the fact that Zika virus has not been eradicated, new outbreaks of Zika can occur anytime.
We are continuing our research to understand how Zika disrupts the development of the fetus, treatment strategies for babies affected by the virus, and ways to prevent Zika infection in the first place. Only when we have a thorough understanding of Zika infections can we assure the health of future generations.
The authors do not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.
Read These Next
How Denver’s Northeast Park Hill community reduced youth violence by 75%
A neighborhood coalition identified risk factors for youth violence and prevention strategies.
2025 was hotter than it should have been – 5 influences and a dirty surprise offer clues to what’s a
Solar cycles, sea ice and rising electricity use all play a role. So does an unhealthy surprise that…
GLP-1 drugs may fight addiction across every major substance, according to a study of 600,000 people
GLP-1 drugs are the first medication to show promise for treating addiction to a wide range of substances.