Applying live bacteria to skin improves eczema
In this clinical trial, the first of its kind, physicians explore whether directly applying a 'good' strain of bacteria to the skin can heal eczema

With two decades of medical education, training, and research under my belt, I have finally reached the stage in my career when I can proudly state that I intentionally spray people in the face with live bacteria.
Atopic dermatitis, more commonly known as eczema, is an inflammatory skin disease that makes skin dry and itchy, causes rashes and leads to skin infections. The cause is unknown, but earlier studies conclude that the skin microbiome – the community of all the bacteria and other microorganisms living on the surface of the skin – plays a major role.
Yet all current eczema treatments ignore the microbiome. Furthermore, almost every current treatment, like topical steroid creams or lotions are time-intensive and must be applied to the skin at least once a day. Other effective treatments such as the Dupixent, which is injected twice per month, requires fewer applications but is extremely expensive. Our team at the National Institutes of Allergy and Infectious Diseases decided to develop a different approach, with the skin microbiome in mind.
Why bacteria?
The first step in looking into whether bacteria could impact eczema was to evaluate past studies that revealed which bacteria make up a healthy skin microbiome. When we compared the locations on the body where patients typically have eczema outbreaks, such as the elbow folds and the back of the knees, with the healthy skin microbiome map, we noticed an intriguing pattern. Body zones prone to symptoms were the same locations where Gram-negative bacteria liked to grow.
Gram staining is a general laboratory method for distinguishing bacteria; Gram-positive organisms like Staphylococcus aureus can separated from Gram-negative organisms like Escherichia coli. The primary reason to separate these types of bacteria is to help physicians understand which types of bacteria are present on a person, so they can select the most effective antibiotic.
We suspected that having the “wrong” kind of Gram-negative bacteria on the skin could lead to eczema. To test the hypothesis we used one particular strain of Gram-negative bacteria, Roseomonas mucosa, collected from the skin of healthy people, to see whether this microbe would calm irritated skin.
We studied R. mucosa in petri dishes, and discovered that it directly killed Staphylococcus aureus– a nasty species of bacteria that is common to skin infections, increases inflammation, and worsens symptoms. In mice, R. mucosa from healthy humans improved the barrier function of the mouse’s skin – the ability to seal in moisture so the skin does not get dry, and the ability to keep allergens like pollen out to protect against becoming allergic. The microbe also improved eczema-like rashes in mice.
Good versus bad bacteria
In humans, R. mucosa boosted the immune system in human skin cells. In contrast, when R. mucosa was collected from people with atopic dermatitis and tested in the same manner, it had no impact or made the eczema worse. This suggests that replacing “bad” strains of R. mucosa with “good” ones might be the key to treating patients.
What distinguishes the “bad” strains of R. mucosa from the bad? That’s a tricky question. To date we have learned that “bad” strains of R. mucosa produce skin irritants – specifically the histamine relative, histidinol, and monomethylgluterate. In contrast, the “good” bacteria make fatty molecules, lipids, that are known to protect the skin from dryness and S. aureus. It appears that the “good” and bad" the strains differ due to subtle changes in their DNA, but more research is needed.
What we do know is that it appears that all the R. mucosa found on healthy people is the “good” kind, while all the R. mucosa on eczema patients is “bad.” While some of the molecular details separating R. mucosa strains are unclear, our results gave us enough actionable information to design an early stage clinical trial to assess the safety and efficacy of applying a mix of three live R. mucosa strains collected from the skin of healthy volunteers and proven to be “good.”
This was the first study to ever evaluate if directly treating the bacteria on the skin could improve skin disease.
Microbial medicines
As part of a small Phase I/II trial, we treated patients who suffer from eczema with a spray containing sugar water and live R. mucosa. First, 10 adults applied the bacteria twice a week for six weeks.
The most important finding was that no one suffered any complications. However, the most exciting discovery was that the majority of participants noticed that their rash and itch subsided. Some reported needing fewer topical steroid applications to control their symptoms. After the adults completed the study, we enrolled five children aged 9 to 14 years.
Just like in adults, no one suffered ill effects and most saw their eczema improve. These kids then reduced the number of days they needed to use topical creams. The bacteria treatment also reduced the population of S. aureus.
Seeing such profound results left me with a mixture of emotions. On one hand, it was extremely gratifying to hear patients and parents relay how much better they or their children felt and to see such amazing differences in both their skin and disposition after treatment.
However, no one on our team, myself included, could feel fully satisfied seeing the disappointment in the patients for whom the treatments failed. Every volunteer expressed enjoyment in participating in the study, learning about their disease, and contributing the medical knowledge. However, anything less than 100 percent improvement in 100 percent of patients suggests we still have more work to do.
Probiotics for the skin?
Since our results support the growing understanding that disruptions in the bacterial balance on the skin directly contribute to eczema, we also explored whether chemicals in common skin care products might aggravate the condition by altering the growth of R. mucosa or S. aureus. Many products with parabens, a common preservative in cosmetics and soaps, and select topical moisturizers, blocked the growth of helpful R. mucosa from healthy skin but did not have the same effects on the growth of S. aureus or eczema-linked R. mucosa. These findings imply that certain products may worsen atopic dermatitis by blocking the growth of the protective R. mucosa.
By using this approach, we hope to offer a way to reduce symptoms and the need for daily treatment – at a reasonable cost. If the good bacteria are capable of colonizing the skin and making it their home, then there is a chance that these microbes could provide long-term benefits long after active treatment stops.
This first phase of our study involved just 15 patients. But based on our results, we plan to launch a bigger trial, likely to include hundreds of patients, to gauge the power of this new treatment. And just as you now buy yogurts that adjust the types and numbers of bacteria in your gut to improve your digestive health, it’s conceivable that we will be using probiotic skin creams to boost the health of the body’s largest organ, the skin.
Ian Myles receives funding from The National Institutes of Health intramural program.
Read These Next
Hezbollah − degraded, weakened but not yet disarmed − destabilizes Lebanon once again
Hezbollah’s entry into the current war followed the killing of Ayatollah Ali Khamenei. The group has…
Housing First helps people find permanent homes in Detroit − but HUD plans to divert funds to short-
Detroit’s homelessness response system could lose millions of dollars in federal funding for permanent…
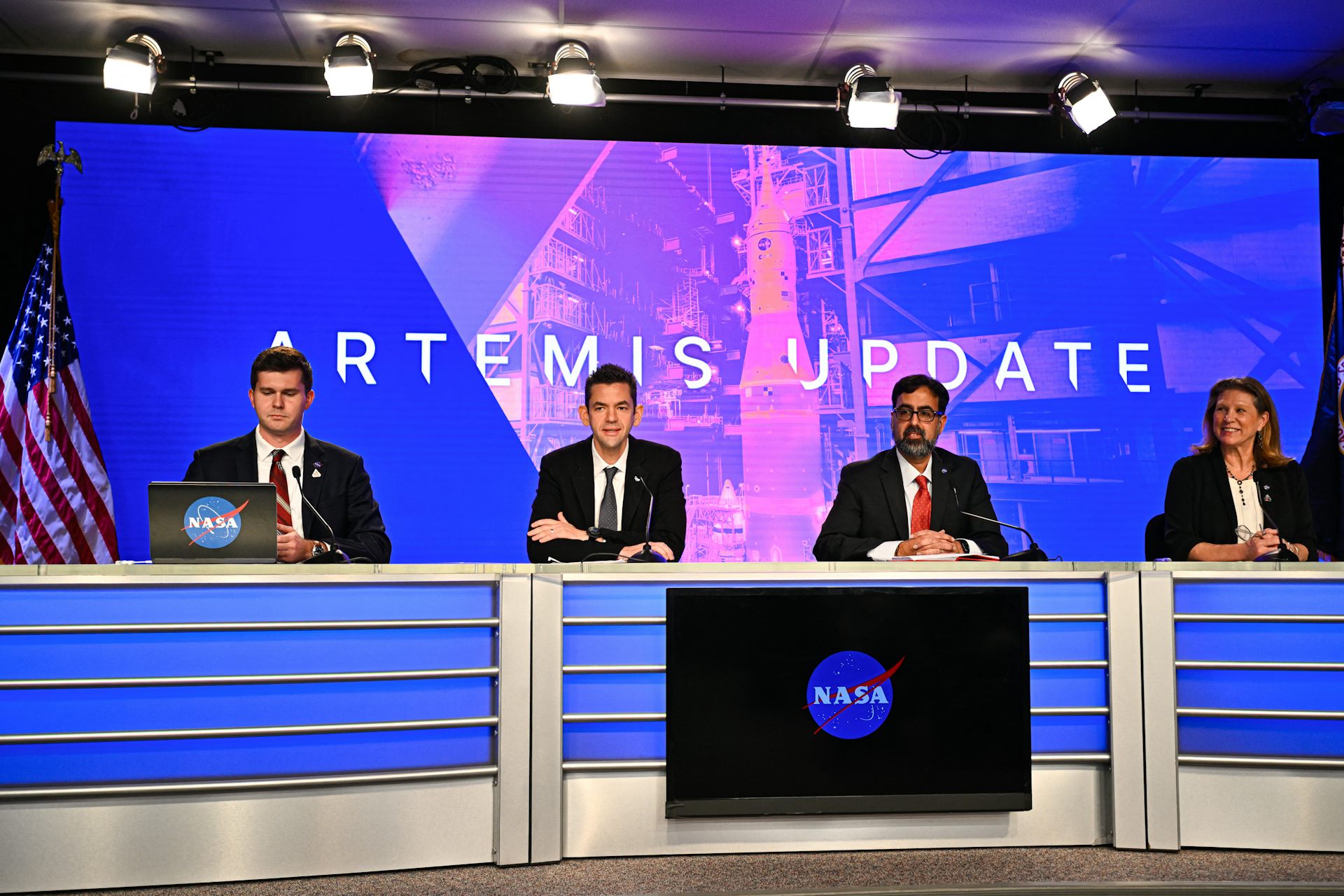
With Artemis II facing delays, NASA announces big structural changes to the lunar program
Artemis II has been plagued by similar issues to those faced by its predecessor, leading NASA to shake…