The deadliest drug in America at center of VA nominee withdrawal: Alcohol
Opioid addiction is a serious public health problem, killing more than 42,000 people a year and ruining families. But alcohol is still the deadliest drug in the US. An addiction expert tells why.

For the first time in a while, pundits and politicians were talking about the drug that kills more people than any other each year in the U.S.
I’m talking about alcohol, which upstaged opioid abuse in news coverage recently, but only after Rear Adm. Ronny L. Jackson withdrew his name for consideration to head Veterans Affairs, in part because of allegations that he has abused alcohol. Jackson has denied any problem with alcohol.
This provides an opportune time to discuss the seriousness of alcohol abuse.
Alcohol contributes to 88,000 deaths in the U.S. each year, more than double the number of people, 42,000, killed by heroin and opioid prescription drug overdose in 2016. Excessive drinking accounted for one in 10 deaths among working-age adults.
In addition, more than 66.7 million Americans reported binge drinking in the past month in 2015, according to a report by the surgeon general.
As someone who has studied alcohol use disorder for over 15 years and who has treated thousands of patients who have it, I think it’s a major, yet often poorly understood, public health problem.
A social lubricant
Alcohol can be a quick and easy way to get into the spirit of a celebration. And it feels good. After two glasses of wine, the brain is activated through complex neurobiochemical processes that naturally release dopamine, a neurotransmitter of great importance.
When the dopamine molecule locks on to its receptor located on the surface of a neuron, or basic brain cell, a “buzz” occurs. It is often desirably anticipated before the second glass is empty.

There are those, however, who drink right past the buzz into intoxication and, often, into trouble. For them, the brain starts releasing the same enjoyable dopamine, no different than what happens in the casual drinker’s, but it doesn’t stop there. A compulsion to binge drink can result.
Binge drinking, defined as drinking five or more drinks for men and four for women on the same occasion on at least one day in the past 30 days, is a medical condition that victimizes the comparative malfunction of the pleasure circuits in the brain.
The three stages of addiction
The alcohol addiction process involves a three-stage cycle: binge-intoxication, withdrawal-negative affect, and preoccupation-anticipation.
It begins in the neurons, the basic type of brain cell. The brain has an estimated 86 billion of these cells, which communicate through chemical messengers called neurotransmitters.
Neurons can organize in clusters and form networks in order to perform specific functions such as thinking, learning, emotions and memory. The addiction cycle disrupts the normal function of some of these networks in three areas of the brain – the basal ganglia, the extended amygdala and the prefrontal cortex.
The disruptions do several things that contribute to continued drinking. They enable drinking-associated triggers, or cues, which lead to seeking alcohol. They also reduce the sensitivity of the brain systems, causing a diminished experience of pleasure or reward, and heighten activation of brain stress systems. Last, they reduce function of brain executive control systems, the part of the brain that typically helps make decisions and regulate one’s actions, emotions and impulses.
These networks are critical for human survival. Unfortunately for the binge drinker, they become “hijacked,” and the bingeing continues even after the harmful effects have begun.
Because binge drinkers’ brains feel intense pleasure from alcohol, there is a powerful motivation to binge drink again and again. What may begin as social binge drinking at parties for recreation can cause progressive neuro-adaptive changes in brain structure and function. The brain is no longer well enough to function normally. Continued partying can transition into a chronic and uncontrollable daily pattern of alcohol use. These maladaptive neurological changes can persist long after the alcohol use stops.
Your brain on alcohol
During the binge-intoxication stage, the basal ganglia rewards the drinker with pleasurable effects, releasing dopamine, the neurotransmitter responsible for the rewarding effects of alcohol and creating the desire for more.
With continued bingeing, the “habit circuity” is repeatedly activated in another part of the basal ganglia called the dorsal striatum. It contributes to the compulsive seeking of more alcohol. This explains the craving that is triggered when a binge drinker is driving by a favorite bar and can’t resist pulling in, even after a promise to go directly home after work.
During the withdrawal-negative affect stage, there is a break from drinking. Because the reward circuit has a diminished ability to deliver a dopamine reward, there is far less pleasure with natural, safe experiences such as food and sex, compared to alcohol.
During abstinence from alcohol, stress neurotransmitters such as corticotropin-releasing factor and dynorphin are released. These powerful neurochemicals cause negative emotional states associated with alcohol withdrawal. This drives the drinker back to alcohol to gain relief and attempt to reestablish the rewards of intoxication.
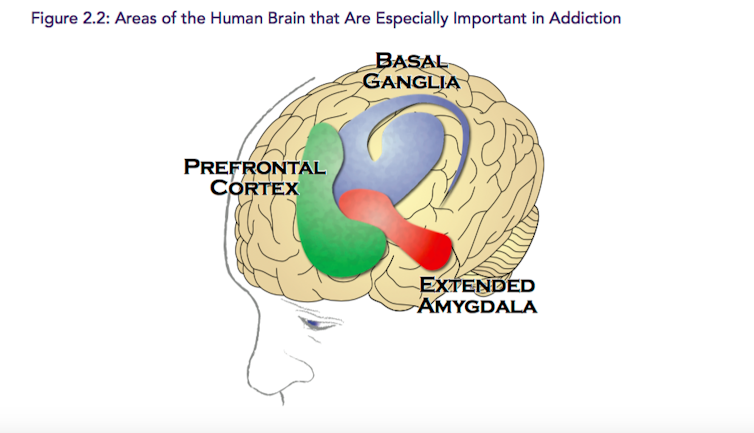
After a period of abstinence from alcohol, which may last only hours, the drinker enters the preoccupation-anticipation stage. This involves the prefrontal cortex, where executive decisions are made about whether or not to override the strong urges to drink. This part of the brain functions with a “go system” and “stop system.”
When the go circuits stimulate the habit-response system of the dorsal striatum, the drinker becomes impulsive and seeks a drink, perhaps even subconsciously. The stop system can inhibit the activity of the go system and is important especially in preventing relapse.
Brain imaging studies show that binge drinking can disrupt the function in both the go and stop circuits. This interferes with proper decision-making and behavioral inhibition. The drinker is both impulsive and compulsive.
An illness that can be treated
Scientific evidence shows that this disorder can be treated.
The FDA has approved three medications for treatment that should be offered whenever appropriate. There is well-supported scientific evidence that behavioral therapies can be effective treatment. This includes recovery support services, such as Alcoholics Anonymous.
Most importantly, it is important to know that alcohol use disorder is a brain disorder causing a chronic illness. It is no different from diabetes, asthma or hypertension. When comprehensive, continuing care is provided, the recovery results improve, and the binge drinker has the hope of remaining sober as long as lifelong treatment and maintenance of sobriety become a dedicated lifestyle choice.
Jamie Smolen does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Read These Next
GLP-1 drugs may fight addiction across every major substance, according to a study of 600,000 people
GLP-1 drugs are the first medication to show promise for treating addiction to a wide range of substances.
Hezbollah − degraded, weakened but not yet disarmed − destabilizes Lebanon once again
Hezbollah’s entry into the current war followed the killing of Ayatollah Ali Khamenei. The group has…
Congress once fought to limit a president’s war powers − more than 50 years later, its successors ar
At the tail end of the Vietnam War, Congress engaged in a breathtaking act of legislative assertion,…






