COVID-19 mRNA vaccines could unlock the next revolution in cancer treatment – new research
The researchers found that mRNA-based COVID-19 vaccines could potentially help patients whose tumors don’t respond well to traditional immunotherapy.
The COVID-19 mRNA-based vaccines that saved 2.5 million lives globally during the pandemic could help spark the immune system to fight cancer. This is the surprising takeaway of a new study that we and our colleagues published in the journal Nature.
While developing mRNA vaccines for patients with brain tumors in 2016, our team, led by pediatric oncologist Elias Sayour, discovered that mRNA can train immune systems to kill tumors – even if the mRNA is not related to cancer.
Based on this finding, we hypothesized that mRNA vaccines designed to target the SARS-CoV-2 virus that causes COVID-19 might also have antitumor effects.
So we looked at clinical outcomes for more than 1,000 late-stage melanoma and lung cancer patients treated with a type of immunotherapy called immune checkpoint inhibitors. This treatment is a common approach doctors use to train the immune system to kill cancer. It does this by blocking a protein that tumor cells make to turn off immune cells, enabling the immune system to continue killing cancer.
Remarkably, patients who received either the Pfizer or Moderna mRNA-based COVID-19 vaccine within 100 days of starting immunotherapy were more than twice as likely to be alive after three years compared with those who didn’t receive either vaccine. Surprisingly, patients with tumors that don’t typically respond well to immunotherapy also saw very strong benefits, with nearly fivefold improvement in three-year overall survival. This link between improved survival and receiving a COVID-19 mRNA vaccine remained strong even after we controlled for factors like disease severity and co-occurring conditions.
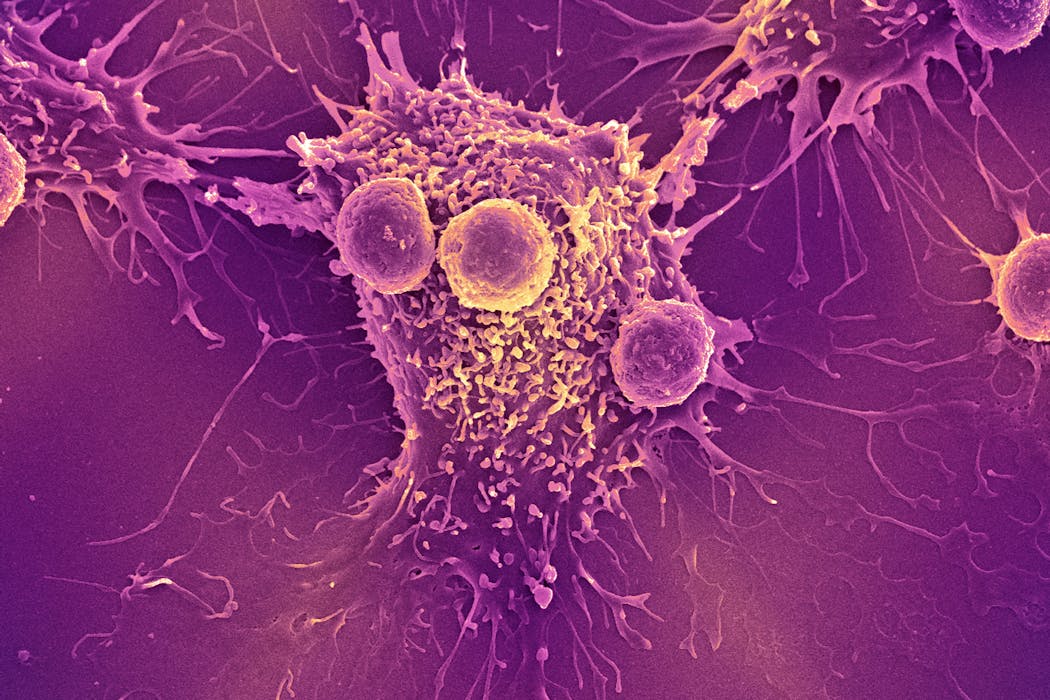
To understand the underlying mechanism, we turned to animal models. We found that COVID-19 mRNA vaccines act like an alarm, triggering the body’s immune system to recognize and kill tumor cells and overcome the cancer’s ability to turn off immune cells. When combined, vaccines and immune checkpoint inhibitors coordinate to unleash the full power of the immune system to kill cancer cells.
Why it matters
Immunotherapy with immune checkpoint inhibitors has revolutionized cancer treatment over the past decade by producing cures in many patients who were previously considered incurable. However, these therapies are ineffective in patients with “cold” tumors that successfully evade immune detection.
Our findings suggest that mRNA vaccines may provide just the spark the immune system needs to turn these “cold” tumors “hot.” If validated in our upcoming clinical trial, our hope is that this widely available, low-cost intervention could extend the benefits of immunotherapy to millions of patients who otherwise would not benefit from this therapy.

What other research is being done
Unlike vaccines for infectious diseases, which are used to prevent an infection, therapeutic cancer vaccines are used to help train the immune systems of cancer patients to better fight tumors.
We and many others are currently working hard to make personalized mRNA vaccines for patients with cancer. This involves taking a small sample of a patient’s tumor and using machine learning algorithms to predict which proteins in the tumor would be the best targets for a vaccine. However, this approach can be costly and difficult to manufacture.
In contrast, COVID-19 mRNA vaccines do not need to be personalized, are already widely available at low or no cost around the globe, and could be administered at any time during a patient’s treatment. Our findings that COVID-19 mRNA vaccines have substantial antitumor effects bring hope that they could help extend the anti-cancer benefits of mRNA vaccines to all.
What’s next
In pursuit of this goal, we are preparing to test this treatment strategy in patients with a nationwide clinical trial in people with lung cancer. People receiving an immune checkpoint inhibitor will be randomized to either receive a COVID-19 mRNA vaccine during treatment or not.
This study will tell us whether COVID-19 mRNA vaccines should be included as part of the standard of care for patients receiving an immune checkpoint inhibitor. Ultimately, we hope that this approach will help many patients who are treated with immune therapy, and especially those who currently lack effective treatment options.
This work exemplifies how a tool born from a global pandemic may provide a new weapon against cancer and rapidly extend the benefits of existing treatments to millions of patients. By harnessing a familiar vaccine in a new way, we hope to extend the lifesaving benefits of immunotherapy to cancer patients who were previously left behind.
The Research Brief is a short take on interesting academic work.
Adam Grippin receives funding from the National Cancer Institute (NCI), the American Brain Tumor Association, and the Radiological Society of North America. He is an inventor on patents related to mRNA therapeutics that are under option to license by iOncology. He is currently employed by the MD Anderson Cancer Center and consults for Sift Biosciences.
Christiano Marconi works for the University of Florida. He receives funding from the UF Health Cancer Center.
Read These Next
GLP-1 drugs may fight addiction across every major substance, according to a study of 600,000 people
GLP-1 drugs are the first medication to show promise for treating addiction to a wide range of substances.
Hezbollah − degraded, weakened but not yet disarmed − destabilizes Lebanon once again
Hezbollah’s entry into the current war followed the killing of Ayatollah Ali Khamenei. The group has…
Housing First helps people find permanent homes in Detroit − but HUD plans to divert funds to short-
Detroit’s homelessness response system could lose millions of dollars in federal funding for permanent…






