Acute stress and early signs of PTSD are common in firefighters and other first responders − here’s
Feelings of sadness or irritability that last a month or more after a life-threatening event could be signs of acute stress or PTSD.

The thousands of firefighters and other first responders on the front lines of the fires that are raging in the Los Angeles area are at increased risk for anxiety, depression, acute stress and post-traumatic stress disorder.
Amanda Mascarelli, The Conversation U.S.’s senior health and medicine editor, spoke with Ian H. Stanley, a clinical psychologist and emergency medicine researcher, about the early signs of acute stress or PTSD and how you can help if a loved one is experiencing these symptoms.
How does PTSD differ in the short term versus the long term?
Post-traumatic stress disorder, or PTSD, is a mental health condition that develops following exposure to a life-threatening event such as a wildfire, a car accident, physical assault or combat. It involves the development of characteristic symptoms that are brought on or that worsen following the trauma and that persist for at least a month.
The symptoms range from nightmares to reliving the event to feelings of guilt and hopelessness or of hypervigilance, meaning constantly being on guard for future threats. Symptoms may also involve sleep disturbances, as well as avoiding certain triggers or reminders of the event. One other important point is that those symptoms must also involve considerable distress or some level of impairment in someone’s life, such as interrupting relationships, work, school or self-care, for instance.
What are potential early signs of acute stress or PTSD?
In this acute phase, as first responders are working the fires, although it’s incredibly stressful, they are trained to put their heads down and push through really difficult events. That doesn’t mean they won’t be affected by it, but in the immediate phase you might not see a lot of symptoms.
But that doesn’t mean they might not then go on to develop symptoms, such as feelings of sadness, irritability or persistent sleep disturbances. Over the longer term, some may develop post-traumatic stress disorder. So, it’s important that people remain vigilant to their mental health and that of others around them.
The biggest things to look out for are any kind of notable changes. There is a wide range of how people experience and react to trauma, and so there’s no concrete formula. Being vigilant to notable changes in others is critical. For example, is someone eating more or less? Are they sleeping more or less? Are they getting cranky more than they used to? Are they drinking more alcohol? And are they hanging out with friends less? Are they engaging less in activities they used to enjoy? If you notice someone is experiencing these types of changes, reach out to them and offer support.
One of the reasons that PTSD symptoms are so worrisome is that it is one of the few mental health conditions that can be very reliably predictive of suicidal thoughts and behaviors. So it’s really important to catch the signs early to prevent the progression.

What about other signs of stress that are different than PTSD?
It’s important to emphasize that it’s normal for people to be sad, angry and anxious following a disaster or other traumatic event.
That said, there is a mental health condition called acute stress disorder that is much like PTSD. Whereas PTSD symptoms need to have existed for at least one month, acute stress disorder can be diagnosed when symptoms last for at least three days and up to one month after a traumatic exposure. In these cases, a person might be experiencing symptoms such as nightmares, persistent negative mood, irritability, sleep disturbances or related conditions.
This diagnosis opens up the opportunity for certain treatments that are reimbursed by insurance and certain pathways for services. Many people with acute stress disorder experience temporary stress responses that do not progress to PTSD; however, about half of individuals with PTSD initially experience acute stress disorder.
Do early symptoms of PTSD always translate to long-term ones?
This is a really important question. When someone’s world as they’ve known it is torn apart and turned upside down – such as in the case with the fires in Southern California – it’s normal to expect changes in the way people think, feel or act. Sadness is normal. Anxiety is normal. Most people who experience these changes get better in a few weeks, and most people do not develop mental health conditions such as PTSD.
There are many different courses that people take with their symptoms. Many people get better with time. Time is a great healer – and so is social support.
But if symptoms persist, reaching out to a mental health professional is critical.
First responders have a higher prevalence of PTSD than the general population. Up to 20% of first responders to natural disasters such as wildfires may go on to develop PTSD.
Importantly, if the firefighter is working in the community in which they live, and they are also affected in their personal life, that’s going to increase their risk.
What treatment options are there for PTSD?
There are very good treatments that work, and PTSD does not have to be a life sentence. Treatment options include medication and psychotherapy. Some people may benefit from mobile health applications, such as “PTSD Coach,” which is freely accessible.
The National Center for PTSD, which is part of the Department of Veterans Affairs, also has helpful resources for family members and loved ones of someone who may be experiencing PTSD.
Ian H. Stanley receives research grant funding from the US Department of Defense, US Centers for Disease Control and Prevention, Face the Fight Foundation, Rutgers University, and Patient-Centered Outcomes Research Institute.
Read These Next
I study why zebrafish larva prefer to circle left or right, to understand how and why human brains e
Being left- or right-handed – and the paw, eye, fin and wing equivalents – is a product of genes,…
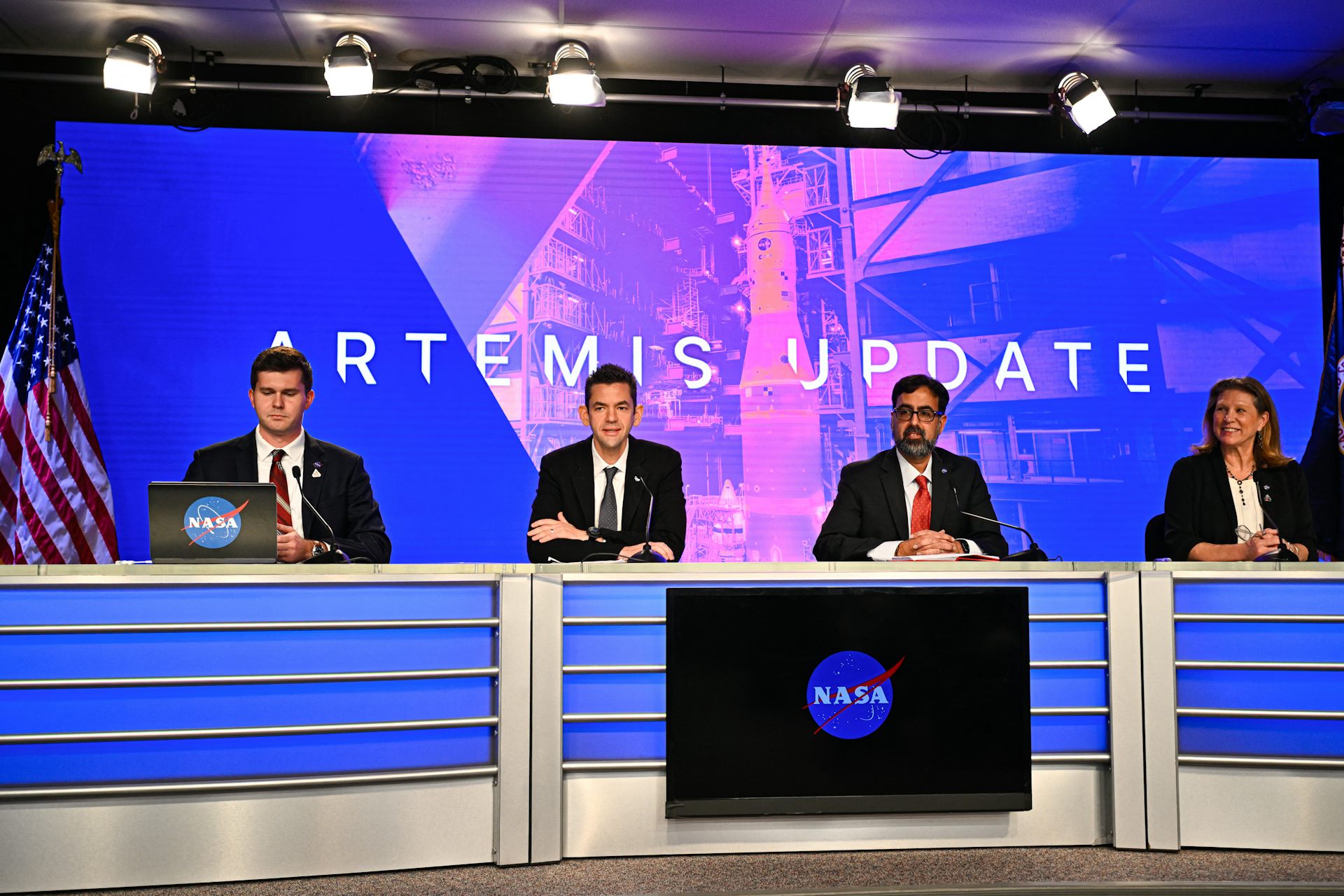
With Artemis II facing delays, NASA announces big structural changes to the lunar program
Artemis II has been plagued by similar issues to those faced by its predecessor, leading NASA to shake…
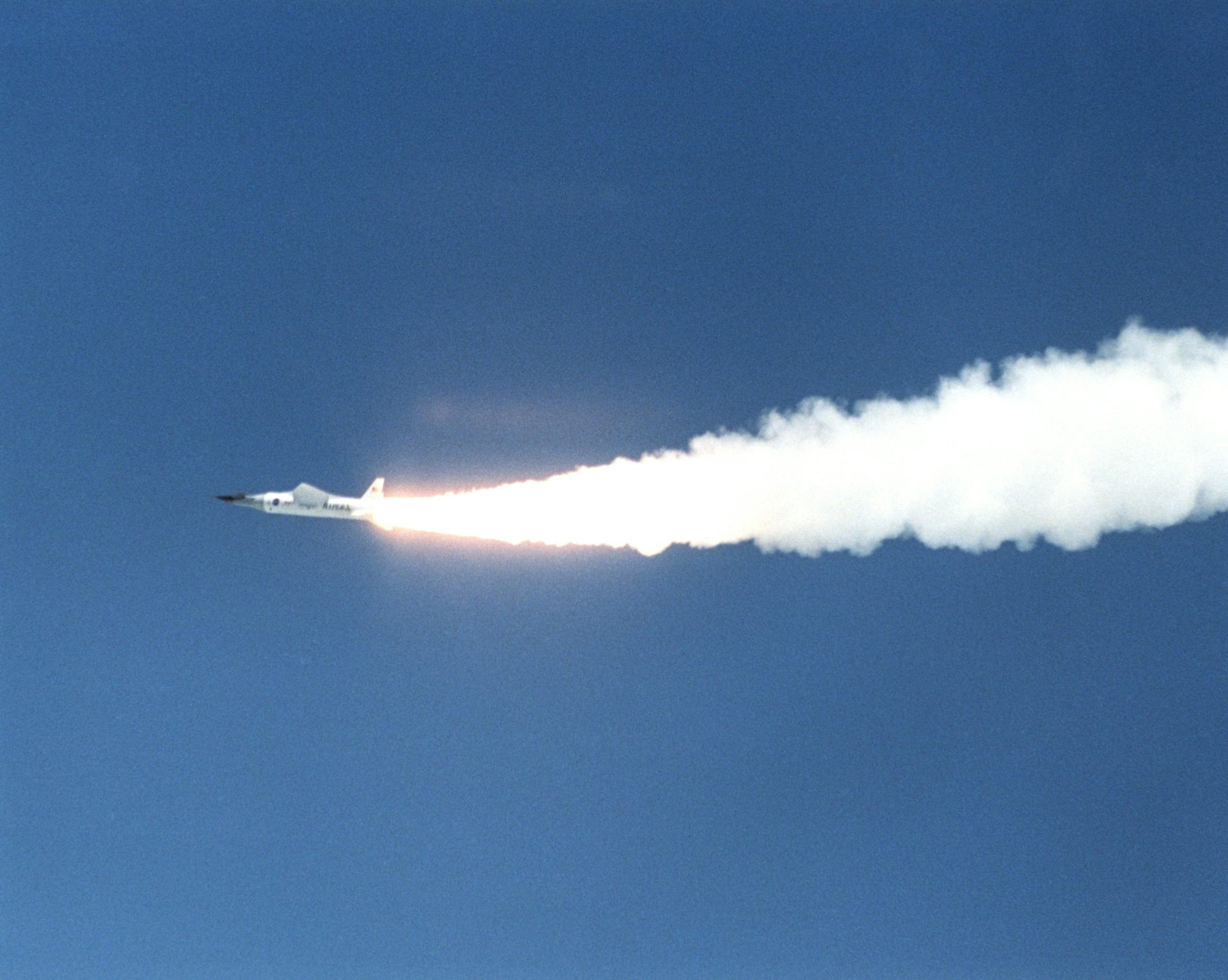
AI and 3D printing help researchers create heat- and pressure-resistant materials for aerospace and
AI models are designing new metal alloys that have been 3D-printed and tested in the lab. The results…