Getting a good night’s rest is vital for neurodiverse children – pediatric sleep experts explain why
Sleep habits can be improved by making shifts in both daytime and evening routines.

Most of us are all too familiar with the consequences of a poor night’s sleep – be it interrupted sleep or simply too little of it. If you’re a parent with kids at home, it often leaves you and your children on edge.
Children with neurodiverse conditions, such as autism and attention-deficit/hyperactivity disorder, or ADHD, are even more susceptible to the effects of poor sleep, given their emotional reactivity and impulsivity.. Struggles with sleep have been linked to increased aggression, irritability, inattention and hyperactivity in children with autism spectrum disorder.
We are three sleep experts – a neurology physician with expertise in pediatrics, a psychologist and a pediatric nurse practitioner – who are working together to help neurodiverse kids, including those on the autism spectrum, get better sleep. Two of us wrote a 2014 book for parents on the topic.
We are passionate about improving sleep because it’s an opportunity to help neurodiverse kids and their families both at night and throughout the day to improve how they function in the world.
The science behind sleep difficulties
There are multiple reasons why neurodiverse children don’t sleep well, including medical conditions, biological causes and behavioral and environmental factors.
Medical conditions, such as obstructive sleep apnea or epilepsy, can affect a child’s sleep. Medications that are used to treat medical conditions, such as antidepressants for mood disorders or stimulants for ADHD, can further disrupt sleep.
Biological causes include genes that affect sleep and issues with processing brain chemicals, such as melatonin.
Behavioral and environmental factors, including the common culprits of increased caffeine, too much screen time and too little physical activity, or any combination of these, can also affect sleep.
Neurodiverse children often struggle with understanding what’s expected of them at bedtime and have difficulty transitioning from after-dinner activities to bedtime routines. They also describe having trouble “turning off their brains” when it’s time to go to sleep.
Treating sleep problems
All of these factors can be addressed and treated. A thorough evaluation by the child’s health care provider may reveal a medical cause, or medication, that is interfering with sleep.
Behavioral approaches can make a big difference in improving sleep. These might include:
Changes to daytime habits, including getting lots of morning light and physical activity.
Shifts in evening habits, such as removing all screens (TV, computers, phones, etc.) and establishing calming bedtime routines.
Modifications to how a parent interacts with their child for those families who would like a child to fall asleep and stay asleep independently.
While behavioral approaches can be successful in helping a neurodiverse child sleep, they need to be tailored to the needs of the individual child and their family. It’s important to note that not all families want their children to sleep on their own. For instance, some cultures value a family bed, and in many families, children share a room with one or more siblings or other relatives.
Because there are so many factors that can cause disrupted sleep, addressing sleep problems cannot be a one-size-fits-all approach and should be done in partnership with parents.
Our team has developed a family-centered approach to address sleep problems in neurodiverse children. This involves brief behavioral sleep education, usually in an initial session lasting up to 90 minutes, and two 30-minute follow-up sessions. In this unique care model designed to increase access to sleep care for families, we train clinicians, including behavioral, speech and occupational therapists, to work with parents to put together a personalized plan.
After only four weeks using this approach, we found that children’s sleep patterns improved, as did their behaviors, and that parents reported feeling more competent in their parenting.
The ups and downs of melatonin
Melatonin is a natural substance that is produced in your brain when it becomes dark in the evening. It makes us drowsy and helps set your brain’s internal clock to promote sleep. Melatonin reduces anxiety and calms down an overaroused brain.
Melatonin is one of the most studied supplements for sleep, and carefully designed studies have shown that it is safe and effective, including large retrospective reviews, systematic reviews, and randomized clinical trials.
While behavioral approaches are recommended as a first-line treatment, melatonin can be helpful in jump-starting a behavioral routine.
There are potential downsides to melatonin, though. It is considered a dietary supplement and is not regulated by the U.S. Food and Drug Administration. This makes it hard for parents to tell how much melatonin a pill or gummy contains, let alone what other substances the supplement may include.
In the past several years, there has been an uptick in overdoses of melatonin. In 2021, compared to 2012, the yearly number of overdoses increased 530%, with more than 260,000 overdoses reported.
That report found that, in cases of overdoses, children experienced drowsiness, dizziness, headache, vomiting and more serious side effects, such as low blood pressure and increased heart rate. Although only a small number of overdoses – 1.6% – resulted in serious outcomes, five children required breathing assistance through mechanical ventilation, and two children died. Overdoses can result from children eating a bunch of gummies, or parents not understanding how much melatonin is safe to give.
To help parents sift through all the resources and articles on melatonin on the internet and social media, one of us created a video and wrote several blogs on melatonin safety. These include topics like whether children can become dependent on melatonin supplements over time, whether taking melatonin will delay puberty, whether children might experience side effects from taking melatonin and more.
Promoting healthier sleep
Here are some general tips for helping your child sleep better, regardless of whether they are neurodiverse:
Choose a consistent bedtime and wake time. This consistency will help children’s own natural melatonin kick in.
Make sure bedtime isn’t too early. For example, an 8 p.m. bedtime is too early for most 10-year-olds. Neurodiverse children may struggle to sleep and will become more anxious, which makes going to sleep even harder.
Help your child get natural sunlight in the morning. Morning sunlight sets our brain’s internal clock so that we can fall asleep more easily at bedtime.
Ensure your child is getting physical activity during the day.
Minimize naps longer than one hour, or after 4 p.m. for school-age children. Naps can interfere with going to sleep at night.
Avoid caffeine, including many types of soda, tea and chocolate.
Turn off all screens and smartphones at least 30 minutes before bedtime.
In the evening leading up to bedtime, turn down all lights in the house. Consider using red night lights, if possible. Set any devices to night mode in the evening to limit exposure to blue light.
Create wind-down time in place of screens. Have your child identify an activity they enjoy that is calming and soothing, such as reading a book, coloring or listening to music. If a bath is stimulating, move it to earlier in the evening, such as after dinner.
Help your child learn to fall asleep without needing you or their devices to be there with them. That way, they will settle down on their own at bedtime. And when they wake up throughout the night, since we all wake up in the night, they will be able to go right back to sleep without becoming fully awake.
For more tips, see Autism Speaks for free downloads of brochures and visual aids.
Beth Ann Malow consults for Neurim Pharmaceuticals which makes a prolonged release melatonin product. She also receives funding from the American Academy of Sleep Medicine.
Dr. Susan Nehiley Brasher received funding from the American Academy of Sleep Medicine.
Terry Katz consults for Scioto Biosciences, which works on live bacterial therapeutics and microbiotics for children and adults with autism and GI disorders. She has received funding from the American Academy of Sleep Medicine and Autism Speaks for research on sleep in children with ASD.
Read These Next
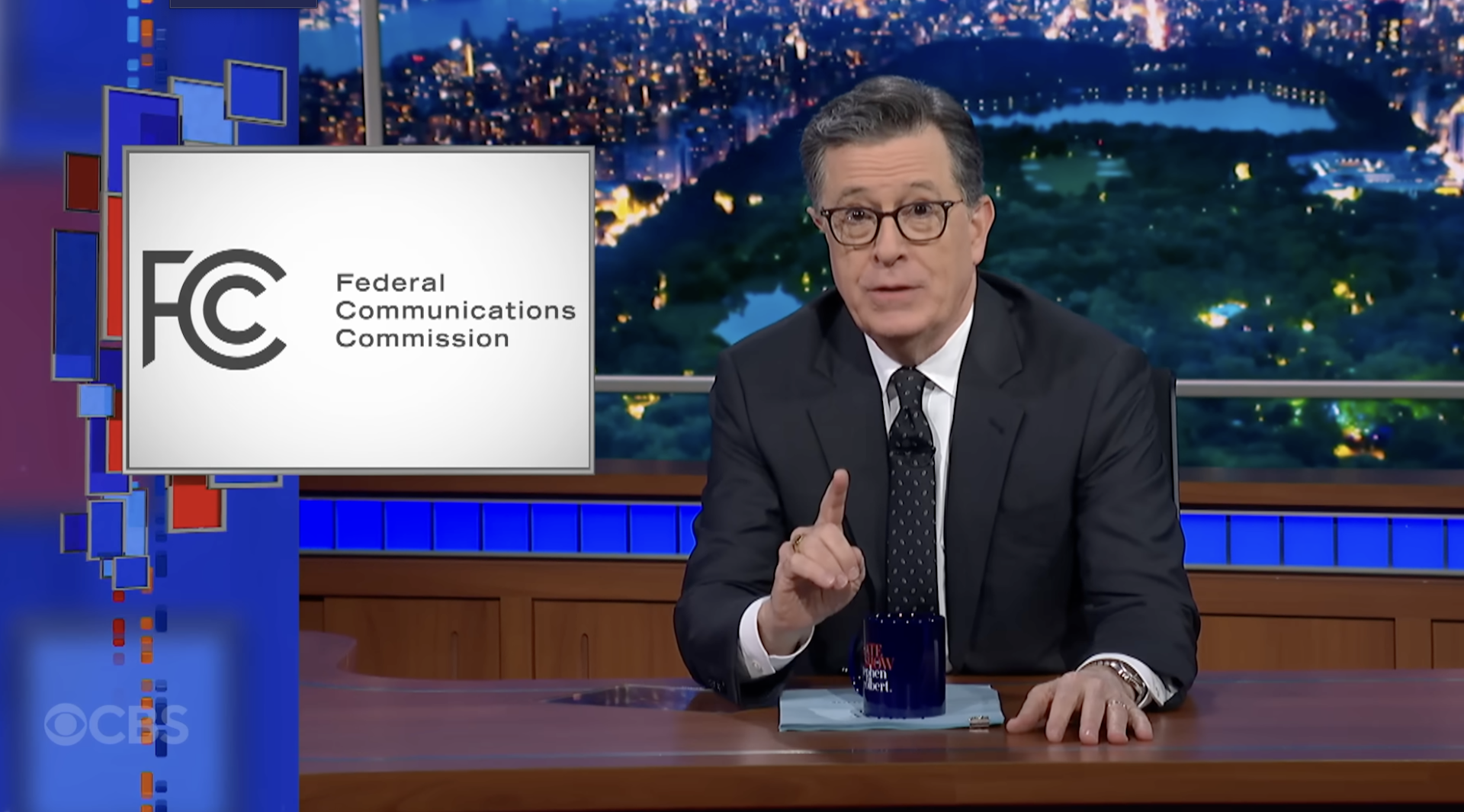
Why Stephen Colbert is right about the ‘equal time’ rule, despite warnings from the FCC
The ‘equal time’ rule has been around for a century and aims to promote broadcasters’ editorial…
As war in Ukraine enters a 5th year, will the ‘Putin consensus’ among Russians hold?
Polling in Russia suggests strong support for President Vladimir Putin. Yet below the surface, popular…
Supreme Court rules against Trump’s emergency tariffs – but leaves key questions unanswered
The ruling strikes down most of the Trump administration’s current tariffs, with more limited options…