Gonorrhea became more drug resistant while attention was on COVID-19 – a molecular biologist explain
The US currently has only one antibiotic available to treat gonorrhea – and it’s becoming less effective.
COVID-19 has rightfully dominated infectious disease news since 2020. However, that doesn’t mean other infectious diseases took a break. In fact, U.S. rates of infection by gonorrhea have risen during the pandemic.
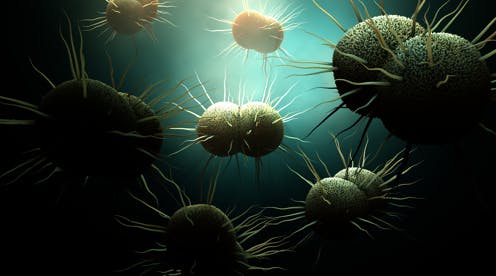
Unlike COVID-19, which is a new virus, gonorrhea is an ancient disease. The first known reports of gonorrhea date from China in 2600 BC, and the disease has plagued humans ever since. Gonorrhea has long been one of the most commonly reported bacterial infections in the U.S.. It is caused by the bacterium Neisseria gonorrhoeae, which can infect mucous membranes in the genitals, rectum, throat and eyes.
Gonorrhea is typically transmitted by sexual contact. It is sometimes referred to as “the clap.”
Prior to the pandemic, there were around 1.6 million new gonorrhea infections each year. Over 50% of those cases involved strains of gonorrhea that had become unresponsive to treatment with at least one antibiotic.
In 2020, gonorrhea infections initially went down 30%, most likely due to pandemic lockdowns and social distancing. However, by the end of 2020 – the last year for which data from the Centers for Disease Control and Prevention is available – reported infections were up 10% from 2019.
It is unclear why infections went up even though some social distancing measures were still in place. But the CDC notes that reduced access to health care may have led to longer infections and more opportunity to spread the disease, and sexual activity may have increased when initial shelter-in-place orders were lifted.
As a molecular biologist, I have been studying bacteria and working to develop new antibiotics to treat drug-resistant infections for 20 years. Over that time, I’ve seen the problem of antibiotic resistance take on new urgency.
Gonorrhea, in particular, is a major public health concern, but there are concrete steps that people can take to prevent it from getting worse, and new antibiotics and vaccines may improve care in the future.
How to recognize gonorrhea
Around half of gonorrhea infections are asymptomatic and can only be detected through screening. Infected people without symptoms can unknowingly spread gonorrhea to others.
Typical early signs of symptomatic gonorrhea include a painful or burning sensation when peeing, vaginal or penal discharge, or anal itching, bleeding or discharge. Left untreated, gonorrhea can cause blindness and infertility. Antibiotic treatment can cure most cases of gonorrhea as long as the infection is susceptible to at least one antibiotic.
There is currently only one recommended treatment for gonorrhea in the U.S. – an antibiotic called ceftriaxone – because the bacteria have become resistant to other antibiotics that were formerly effective against it. Seven different families of antibiotics have been used to treat gonorrhea in the past, but many strains are now resistant to one or more of these drugs.
Why gonorrhea is on the rise
A few factors have contributed to the increase in infections during the COVID-19 pandemic.
Early in the pandemic, most U.S. labs capable of testing for gonorrhea switched to testing for COVID-19. These labs have also been contending with the same shortages of staff and supplies that affect medical facilities across the country.
Many people have avoided clinics and hospitals during the pandemic, which has decreased opportunities to identify and treat gonorrhea infections before they spread. In fact, because of decreased screening over the past two and a half years, health care experts don’t know exactly how much antibiotic-resistant gonorrhea has spread.
Also, early in the pandemic, many doctors prescribed antibiotics to COVID-19 patients even though antibiotics do not work on viruses like SARS-CoV-2, the virus that causes COVID-19. Improper use of antibiotics can contribute to greater drug resistance, so it is reasonable to suspect that this has happened with gonorrhea.
Overuse of antibiotics
Even prior to the pandemic, resistance to antibiotic treatment for bacterial infections was a growing problem. In the U.S., antibiotic-resistant gonorrhea infections increased by over 70% from 2017-2019.
Neisseria gonorrhoeae is a specialist at picking up new genes from other pathogens and from “commensal,” or helpful, bacteria. These helpful bacteria can also become antibiotic-resistant, providing more opportunities for the gonorrhea bacterium to acquire resistant genes.
Strains resistant to ceftriaxone have been observed in other countries, including Japan, Thailand, Australia and the U.K., raising the possibility that some gonorrhea infections may soon be completely untreatable.
Steps toward prevention
Currently, changes in behavior are among the best ways to limit overall gonorrhea infections – particularly safer sexual behavior and condom use.
However, additional efforts are needed to delay or prevent an era of untreatable gonorrhea.
Scientists can create new antibiotics that are effective against resistant strains; however, decreased investment in this research and development over the past 30 years has slowed the introduction of new antibiotics to a trickle. No new drugs to treat gonorrhea have been introduced since 2019, although two are in the final stage of clinical trials.
Vaccination against gonorrhea isn’t possible presently, but it could be in the future. Vaccines effective against the meningitis bacterium, a close relative of gonorrhea, can sometimes also provide protection against gonorrhea. This suggests that a gonorrhea vaccine should be achievable.
The World Health Organization has begun an initiative to reduce gonorrhea worldwide by 90% before 2030. This initiative aims to promote safe sexual practices, increase access to high-quality health care for sexually transmitted diseases and expand testing so that asymptomatic infections can be treated before they spread. The initiative is also advocating for increased research into vaccines and new antibiotics to treat gonorrhea.
Setbacks in fighting drug-resistant gonorrhea during the COVID-19 pandemic make these actions even more urgent.
Kenneth Keiler receives funding from NIH.
Read These Next
Not all mindfulness is the same – here’s why it matters for health and happiness
Mindfulness is taught everywhere, from schools to workplaces. But scientists define and measure it in…
Should medical marijuana be less stringently regulated? A drug policy expert explains what’s at stak
The proposed rescheduling of marijuana could have far-reaching implications in science, medicine and…
Innovations in asthma care can improve the health of Detroiters living with this chronic disease
Detroiters are hospitalized for asthma four times more often than Michigan residents overall. A proactive…





