COVID-19 makes clear that bioethics must confront health disparities
A bioethicist argues that the problem of health disparities existed long before COVID-19 struck with a vengeance in marginalized communities.

With some reluctance, I’ve come to the sad realization the COVID-19 pandemic has been a stress test for bioethics, a field of study that intersects medicine, law, the humanities and the social sciences. As both a physician and medical ethicist, I arrived at this conclusion after spending months at what was once the epicenter of the pandemic: New York City. I was overseeing a 24/7 bioethics consultation service.
I work in a nationally ranked academic medical center in Manhattan. As it did with all hospitals in New York City, COVID-19 put us under tremendous pressure to respond to the surge of patients who came to us for care. In the early days, we struggled with inadequate provisions. Yet we persevered. We increased our ICU capacity by more than 200%, redeployed our clinical workforce in creative ways, and provided a “crisis standard of care.” Simply put, we did the best we could under extreme conditions. In all my years in medicine, I have seen nothing like it. I imagine the only analogy would be practicing medicine on a battlefield.

As challenging as our situation was, colleagues across New York City had it worse. I was especially struck by what hospitals experienced in the boroughs of Queens and the Bronx. Chronically under-resourced, they were also caring for patients who long suffered from the consequences of inadequate primary care. Those with untreated hypertension, diabetes, obesity, and other chronic conditions were especially prone to the ravages of coronavirus. The rows of refrigerator trucks outside a hospital in Elmhurst, Queens, parked there to temporarily hold the dead, was a horrifying symbol of the distress. As a scholar, I try to avoid becoming emotional, but seeing them reminded me, once again, of a battle: specifically, what my Dad had seen as a combat medic in World War II. But this was happening in New York City.
Such images have forced me to question the relevance of bioethics – and ask why my field hasn’t done more to identify these disparities and do something about them. To be sure, my team and I provided ethics consultations in our hospital, and I participated in policy discussions at the institutional and state level. But our focus for the most part was too narrow and ignored a tale of inequity unfolding around us.
One example: Our hospital in Manhattan evacuated patients from hospitals in Brooklyn and Queens to help with their case load. At the state level, there was talk to make things easier by coordinating such transfers. But mostly, the efforts were too little, too late. Inequity was baked into the system long before the pandemic. Nothing could be done to reverse that inequity, once waves of patients flooded the system.
Why hadn’t bioethics done more to anticipate these challenges and mitigate them? The answer is complex, and the history goes back generations.

Bioethics 101
Bioethics, a phrase coined in 1973, was a response to the Nazi atrocities in medicine, the Tuskegee Syphilis Study, and the challenges posed by increasingly sophisticated medical practice. Bioethics called for including the patient’s voice in care decisions, an affirmation of their rights, and a focus on four principles: autonomy, beneficence, non-maleficence and justice.
[You need to understand the coronavirus pandemic, and we can help. Read The Conversation’s newsletter.]
But along the way, one of those principles was prized to the exclusion of the others. A European bioethicist once told me, with irony, that American medicine followed four ethical principles: autonomy and three others he could not recall.
Still, bioethics in the U.S. became something of a rights movement, akin to other civil rights movements of the era. The goal was to minimize hierarchies and give voice to the voiceless. The sanctioning of patient enfranchisement in bioethics was a response to entrenched paternalism (doctor knows best). Notably, it led to the right-to-be-left-alone and the right-to-die movement typified by cases like Karen Quinlan, Nancy Cruzan and Terri Schiavo.
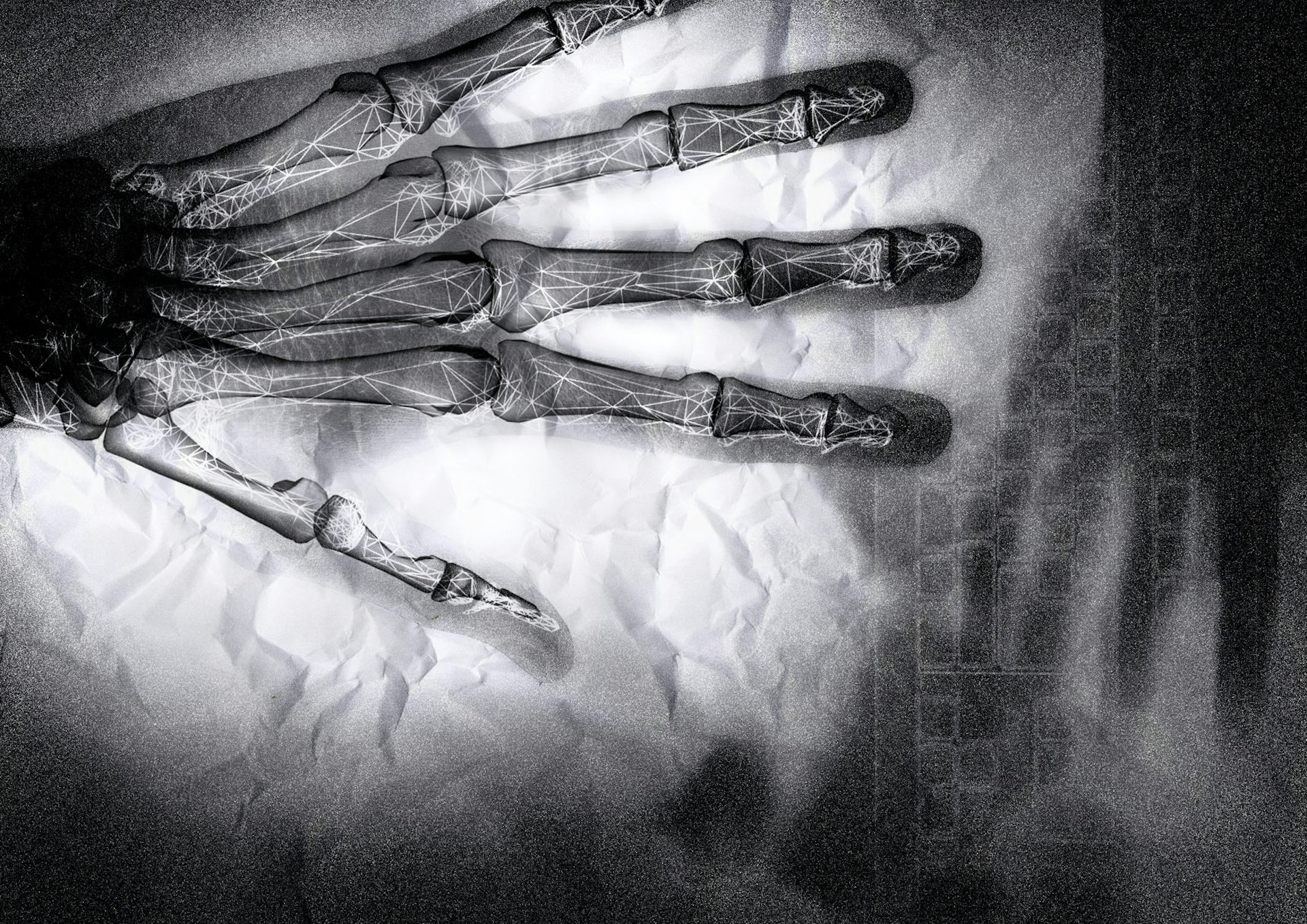
With the elevation of self-determination, the pursuit of the other three principles – the promotion of good, the avoidance of harm, and the passion for social justice – was diminished. These limitations were laid bare by the morbidity and mortality data from the COVID-19 pandemic in New York City. Neighborhoods of color, poverty and poorer educational attainment were hardest hit – those very neighborhoods that had hospitals with an insufficient number of beds and poor access to primary care. The death rate in the Bronx was double that of Manhattan. This was a consequence of poverty, population density and the structural racism in medicine and health policy.
Bioethics needs to move beyond narrow questions of patient choice, particularly when the disenfranchised are not in a position to exercise that choice.
In 2009, as we prepared for an avian flu pandemic that never arrived, I posed these questions in an essay for the Hastings Center Bioethics Forum. I was worried about how entrenched and endemic disparities might compound the malign effects of a pandemic.
At that time, the average number of ventilators was 39.2 per 100,000 people in Manhattan, compared to 14.1 per 100,000 people in Queens. Imagining a pandemic flu, I worried that “rationing ventilators would be especially harsh in Queens” and would lead to “disproportionate death.” This is precisely what happened during the COVID-19 crisis a decade later.
While physicians and health care officials focus on the acute consequences of COVID-19, we must also recognize the real pathology existed long before the pandemic struck. The pre-existing condition of health care disparities led to the disproportionate burden on vulnerable communities from COVID-19.
Now is the time for bioethics to broaden its gaze and appreciate that rights without opportunity ring hollow. The Nobel Laureate Amartya Sen rightly observed the limited utility of negative rights if they did yield just results. Bioethics needs to learn from the COVID-19 experience lest its obsession with midcentury catechisms make it an historical artifact of an earlier era.
Joseph J. Fins does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.
Read These Next
Artists and writers are often hesitant to disclose they’ve collaborated with AI – and those fears ma
Whether they’re famous composers or first-year art students, creators experience reputational costs…
Honoring Colorado’s Black History requires taking the time to tell stories that make us think twice
This year marks the 150th birthday of Colorado and is a chance to examine the state’s history.
When civil rights protesters are killed, some deaths – generally those of white people – resonate mo
From the civil rights era of the 1960s until today, white victims of government violence have received…