Why Amazon should keep prescription drugs off its voluminous shelves
Amazon currently sells pretty much everything, including the kitchen sink, but medications are very different from books and fidget spinners.

Amazon hit a milestone recently after the price of one share hit US$1,000 for the first time, giving it a total value of close to $500 billion. That makes it the fourth-biggest company in the U.S. in terms of market capitalization and twice the size of brick-and-mortar rival Walmart.
The online retailer’s incredible growth has come from expanding into more and more areas of the economy, providing its customers with speedy delivery of everything from socks and books to lawn chairs and computers. One category it has yet to enter, however, is prescription drugs.
Amazon wants to change that and dispense drugs alongside its hundreds of millions of other wares. Would this be a good thing for consumers and the health care system?
The biggest online retailer’s entry into this market may lead to efficiency gains, but the cost would be dear in terms of further severing the link between patients and actual pharmacists. Research, including my own, shows that patients need more face-to-face time with pharmacists, not less.

Brief history of pharmacies
Pharmacies (or apothecaries, as they were once known) have existed since antiquity. The first retail pharmacy began in Philadelphia in 1729. Back then, pharmacists not only dispensed medications to patients (without a prescription) but diagnosed diseases and handcrafted drugs. In 1951, Congress passed the Federal Food, Drug and Cosmetic Act, which prohibited pharmacists from dispensing FDA-approved drugs without a valid prescription.
Mail-order pharmacies harnessing the raw efficiency of mass-filling prescriptions began to boom in the 1980s. In 2013, about 39 percent of customers said they refilled their prescription by mail order, up from an estimated 6 percent in 1990.
Clearly it costs less per unit of labor for prescriptions to be filled in a centralized facility with industrial pill counting technology and with auto-refills of medication than when prescriptions are filled manually in the store by a local pharmacist triggered by a patient calling the pharmacy.
Consumers say they like the convenience of mail-order pharmacies, which is likely one of the reasons Amazon is getting serious about entering the $450 billion market for prescription drugs.
Amazon might be able to enhance the user experience, as well as make the process even more efficient, but there’s a cost.
Drugs aren’t socks
What is missing from the discussion is that prescription drugs are not socks or refrigerators. When consumers take drugs, they become patients, not just customers.
While prescription drugs hold the promise of preventing disease and treating symptoms, they can maim or even kill if not used correctly.
In 1993, for example, medication-related errors led to about 7,400 deaths, more than double the number of fatalities in 1983, according to a review of death certifications. Unfortunately, they’re the latest data available, but most likely the number is higher today.
A key reason for these errors seems to be a lack of communication. A 2003 report noted that better communication among physicians, pharmacists and nurses could prevent 86 percent of the most serious medication errors, which suggests shifting more drug dispensation to a centralized facility from local pharmacies would worsen the problem.
Too many people aren’t taking their meds
Another thing that makes prescription drugs very different than Amazon’s typical offerings is that in many cases it’s essential that patients actually take their meds as prescribed. That’s not happening.
Taking drugs in the right dosage for the right amount of time is critical to effectively cure a disease, prevent the formation of antimicrobial resistance and keep a malady from progressing.
Yet on average, only about 50 percent of American patients typically take their medicines as prescribed, costing hundreds of billions of dollars in adverse outcomes and unnecessary hospitalizations each year.
Furthermore, in my own research involving patients with cardiovascular diseases, I have found that people are simply not receiving the medications they need – and when they are, they aren’t following through on the required dosage, leading to worse outcomes. I’ve found that greater interaction between patients and pharmacists can help solve this problem.
Other studies have shown that more active face-to-face engagement with a pharmacist improves a patient’s level of adherence to a prescription, which can lead to better outcomes. A study involving Walgreens pharmacists, for example, suggested direct drug counseling reduced health care costs by $266 on average, mostly due to fewer hospitalizations.

The environmental costs
Finally, another key aspect of prescription drugs is that their waste is a big and growing problem.
Unlike the clothes or appliances you order, medications can’t simply be returned to the merchant, restocked and resold to another customer. There’s no way of ensuring they weren’t adulterated or improperly stored, and the risks are too great. That means every pill that goes unused must be disposed of, which is a huge waste of money but also is a major source of pollution.
In a 2015 assessment of medications turned in for disposal, more than half of the prescriptions purchased from mail-order pharmacies still contained 80 percent of more of the original pills. Even more troubling, 39 percent had every single pill originally dispensed. That compares with much-lower rates of 37 percent and 17 percent for community pharmacies.
Many of the unused drugs, however, aren’t properly disposed of and instead end up in a landfill or flushed down a toilet.
A nationwide study conducted by the U.S. Geological Survey in 1999 and 2000 found low levels of pharmaceuticals – including antibiotics, hormones, contraceptives and steroids – in 80 percent of the rivers and streams sampled, contaminating 40 million Americans’ drinking water.
Studies have shown that aquatic animals are adversely affected by these hormones, with some male fish developing female sex organs, and there are concerns that long-term exposure to a tainted water supply can lead to more superbugs.

Small gains for many pains
Amazon is a revolutionary company that has reshaped how we shop and has helped drastically increase the efficiency of shipping small packages. This could even allow it to reduce some of the negative side effects, noted above, of remote pharmacies, such as by making it more cost-effective to ship small quantities of pills to reduce waste.
But to my mind, any modest gains in efficiencies or cost savings are paid for dearly by the negative outcomes that result from medication-related errors and patients not following through on their prescriptions, while the waste of unused drugs will continue. And while this problem has been with us for a while, Amazon, due to its size and ability to quickly dominate markets, would make the situation a lot worse.
Delivering a product more efficiently cannot be the only metric of success. With prescription drugs, saving lives must be considered as well.
C. Michael White does not work for, consult, own shares in or receive funding from any company or organization that would benefit from this article, and has disclosed no relevant affiliations beyond the academic appointment above.
Read These Next
GLP-1 drugs may fight addiction across every major substance, according to a study of 600,000 people
GLP-1 drugs are the first medication to show promise for treating addiction to a wide range of substances.
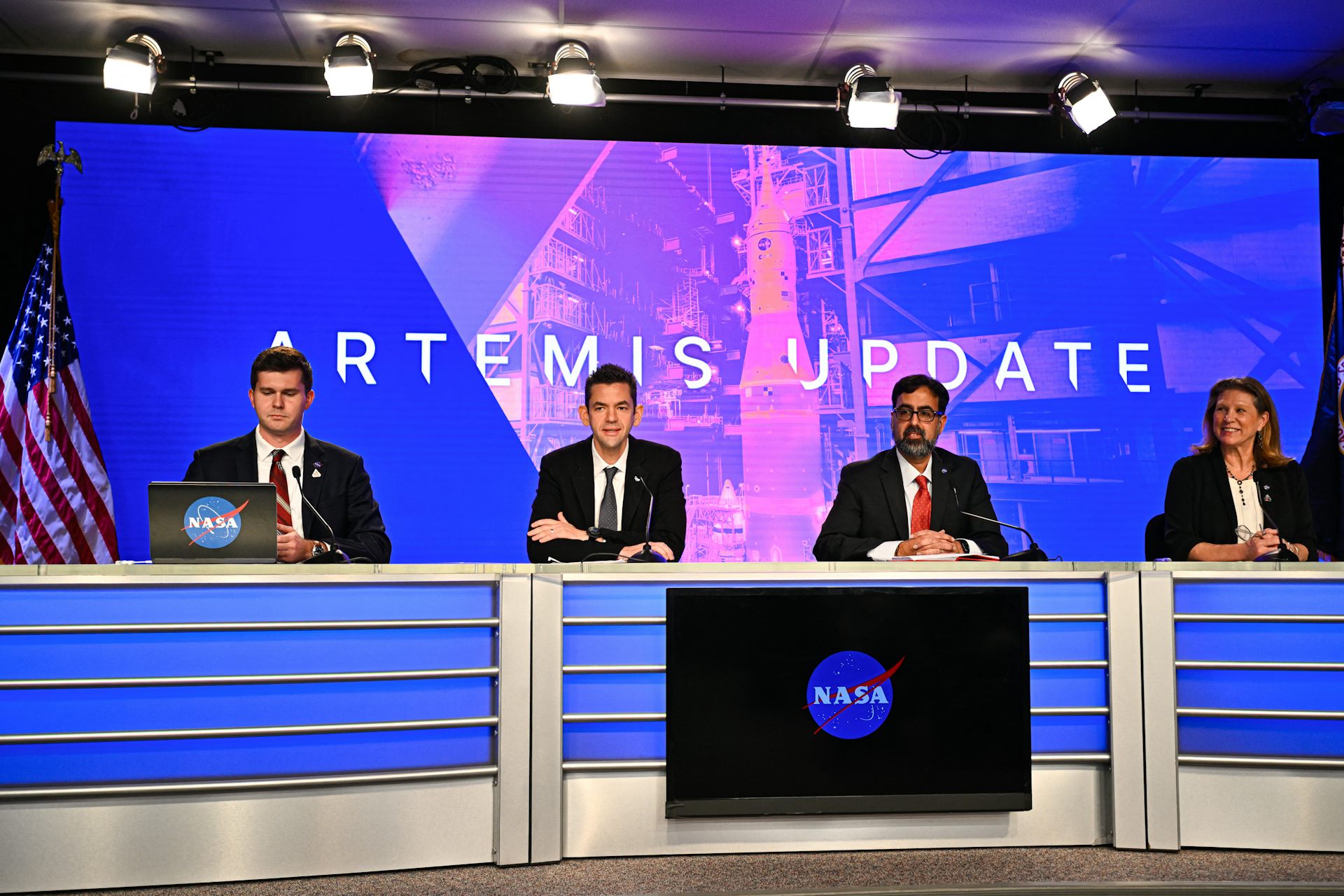
With Artemis II facing delays, NASA announces big structural changes to the lunar program
Artemis II has been plagued by similar issues to those faced by its predecessor, leading NASA to shake…
What decades of research reveal about involuntary substance use treatment – and why evidence points
Many cities are considering involuntary substance use treatment as a solution to drug use among the…